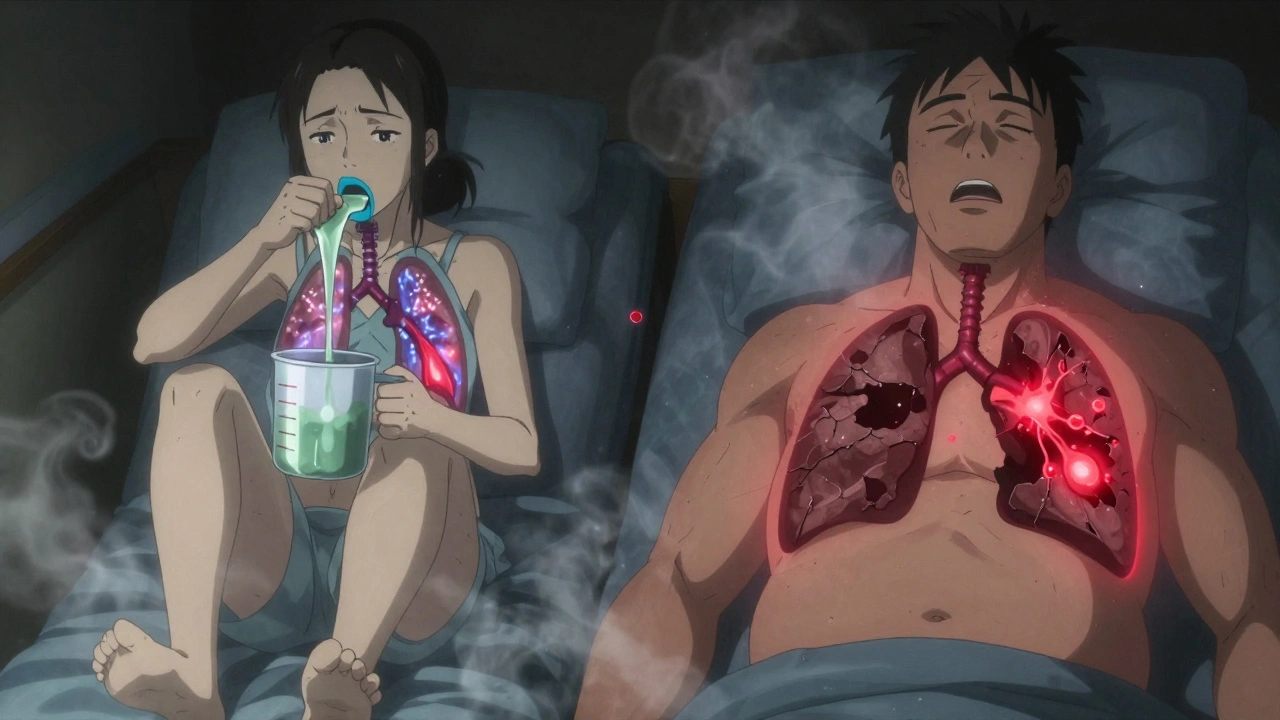
When working with Chronic Bronchitis, a long‑term inflammation of the bronchi that causes persistent cough and mucus production. Also known as chronic bronchitis, it Smoking often fuels the condition and can push it toward COPD. This trio of chronic bronchitis, smoking, and COPD creates a cycle of airway inflammation, mucus hypersecretion, and reduced lung function. Below you’ll find a practical roadmap that ties these pieces together and helps you navigate daily life with the condition.
First, let’s look at why chronic bronchitis shows up. The primary trigger is repeated irritation of the airway lining—most commonly from cigarette smoke, but also from polluted air, occupational dust, or long‑term exposure to chemicals. That irritation ramps up airway inflammation, causing the bronchi to swell and produce excess mucus. Over time the mucus becomes thick, sticky, and hard to clear, leading to the hallmark daily cough that lasts at least three months over two consecutive years. People often notice the cough first in the mornings, followed by wheezing, shortness of breath, and a feeling of heaviness in the chest.
Diagnosing chronic bronchitis is straightforward but requires a thorough look at symptoms and a few tests. Doctors usually start with a detailed history—asking about smoking habits, exposure to irritants, and the pattern of the cough. A physical exam can reveal crackles or wheezing, while spirometry measures lung capacity and helps differentiate chronic bronchitis from other obstructive diseases. In some cases, a chest X‑ray or CT scan confirms the presence of airway thickening and rules out infections.
Now, what can you actually do about it? The cornerstone of management is removing or reducing exposure to the irritants that started the problem. Quitting smoking is the single most effective step; studies show lung function stabilizes within months after cessation, and the cough often lessens. Beyond that, regular physical activity improves airway clearance and boosts overall lung health. Medications such as bronchodilators open the airways, while expectorants thin the mucus, making it easier to cough out. In more severe cases, inhaled steroids may be prescribed to tame inflammation, and pulmonary rehabilitation programs teach breathing techniques that reduce breathlessness.
It’s also worth noting the long‑term outlook. Chronic bronchitis doesn’t always stay isolated; many patients eventually develop chronic obstructive pulmonary disease (COPD), especially if they keep smoking. That progression adds extra challenges—more frequent flare‑ups, higher risk of infections, and greater need for oxygen therapy. However, early intervention, consistent medication use, and lifestyle changes can slow or even halt the shift to COPD. Keeping vaccinations up to date (flu and pneumonia shots) also cuts down on respiratory infections that can worsen symptoms.
In short, chronic bronchitis sits at the intersection of airway inflammation, mucus overload, and harmful inhalants like smoke. By understanding how these elements interact, you can take concrete steps—quit smoking, stay active, and follow a tailored treatment plan—to keep symptoms in check and protect your lungs from further damage. Below you’ll find a curated list of articles that dive deeper into each of these topics, from practical quitting tips to medication comparisons, giving you a full toolbox to manage the condition effectively.