Bronchitis Immune Response Simulator
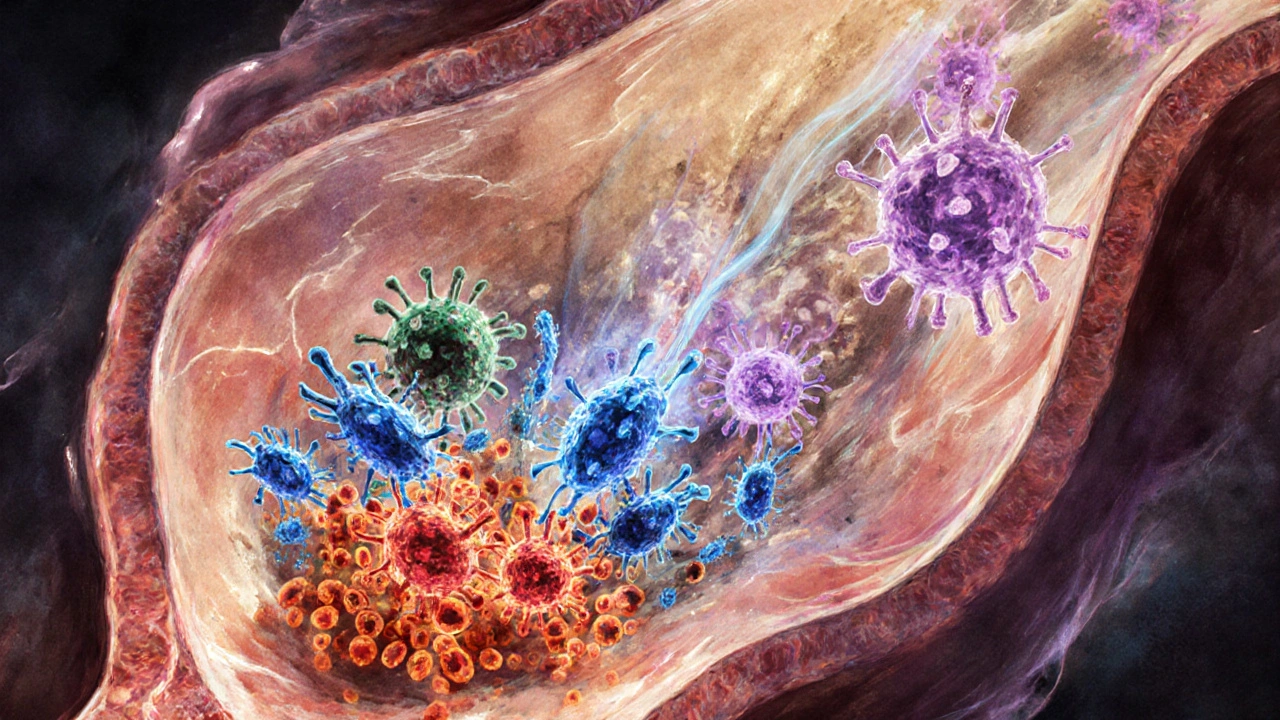
This interactive simulator shows how immune cells fight bronchitis and how lifestyle choices impact your immune response. Try different scenarios to see how your body responds!
Macrophages
Patrol the lungs and engulf pathogens. In acute bronchitis, they activate quickly; in chronic cases, they become overactive.
Neutrophils
Rush to infection sites rapidly. They cause swelling and wet cough in acute cases but contribute to damage in chronic bronchitis.
Lymphocytes
Coordinate long-term immune responses. Key in viral infections, but can cause fatigue during prolonged illness.
Immune Response Summary
Key Takeaways
- Bronchitis is an inflammation of the airways that triggers a specific immune response.
- Acute bronchitis is usually viral and resolves in weeks; chronic bronchitis is linked to long‑term irritants.
- The immune system’s frontline cells-macrophages, neutrophils, and lymphocytes-drive both symptom relief and tissue damage.
- Smoking, air pollution, and poor nutrition weaken immunity and make bronchitis more likely.
- Support the immune system with rest, hydration, vaccines, and targeted supplements while following medical advice.
When you hear the word Bronchitis is a condition where the bronchial tubes become inflamed, swollen, and produce excess mucus, you might picture a persistent cough and a chest that feels tight. What many people don’t realize is how tightly bronchitis is woven into the body’s immune machinery. This article unpacks what happens inside your lungs, why some coughs disappear quickly while others linger, and what practical steps you can take to keep your immune system on your side.
What Exactly Is Bronchitis?
Bronchitis falls under the broader umbrella of respiratory infections. It can be split into two main types:
- Acute bronchitis - a short‑term infection, most often caused by viruses such as influenza or rhinovirus.
- Chronic bronchitis - a long‑lasting condition defined by a productive cough for at least three months a year over two consecutive years, usually linked to smoking or chronic irritant exposure.
Both types involve inflammation the body’s protective response that brings blood, immune cells, and chemicals to an injured area, but the triggers and outcomes differ.
How the Immune System Reacts to Bronchial Irritation
When an invader-be it a virus, bacterium, or pollutant-enters the bronchial tree, the immune system launches a multi‑layered defense:
- Macrophages large white blood cells that patrol the lungs and swallow pathogens settle on the airway lining and attempt to engulf the offending agents.
- Neutrophils fast‑acting immune cells that rush to the infection site and release enzymes to break down microbes arrive within minutes, causing swelling and the classic “wet” cough.
- Lymphocytes cells that coordinate a longer‑term response, producing antibodies or activating other immune pathways become more active in viral infections, helping clear the virus but also contributing to fatigue.
These cells release cytokines signaling proteins that orchestrate inflammation and fever. While cytokines are essential for fighting infection, too much can damage the delicate airway lining, leading to excess mucus, bronchospasm, and the persistent cough that makes bronchitis so uncomfortable.
Acute vs. Chronic: Immune Mechanics Differ
| Feature | Acute Bronchitis | Chronic Bronchitis |
|---|---|---|
| Typical cause | Viral (influenza, RSV) or bacterial | Long‑term irritants (smoking, polluted air) |
| Immune cells dominant | Neutrophils & macrophages - short burst | Macrophage activation & persistent neutrophil influx |
| Cytokine pattern | High IL‑6, TNF‑α early, then taper | Elevated IL‑8, persistent low‑grade inflammation |
| Duration | 1‑3 weeks | Months to years, often irreversible |
| Response to antibiotics | Effective only if bacterial | Limited benefit; focus on bronchodilators & rehab |
In acute bronchitis, the immune system acts like a sprint-fast, intense, then winds down. Chronic bronchitis feels more like a marathon, with the immune system stuck in a low‑grade inflammatory mode that slowly erodes airway function.
Why Some People Get Sick More Frequently
Several lifestyle and biological factors tip the scale toward a weaker immune response:
- Smoking introduces tar and chemicals that impair ciliary movement and immune cell function directly damages the bronchial epithelium.
- Air pollution fine particulate matter (PM2.5) that triggers oxidative stress and inflammation in the lungs weakens the first line of defense.
- Age both very young children and older adults have less robust immune responses making them more vulnerable.
- Chronic stress and poor sleep lower cortisol regulation, decreasing the ability of lymphocytes to proliferate effectively.
- Vitamin D deficiency, common in higher latitudes during winter, reduces antimicrobial peptide production.
Addressing these variables can boost immune resilience and lower the odds of both acute flare‑ups and chronic progression.
Supporting Your Immune System During a Bronchitis Episode
When you’re already coughing, the goal isn’t to overwhelm the immune response but to guide it toward a clean, swift resolution. Here are evidence‑backed actions:
- Rest and hydration - Fluids thin mucus, making it easier for cilia to clear. Rest reduces metabolic stress on immune cells.
- Steam inhalation - Warm, moist air soothes irritated bronchial tissue and improves mucociliary clearance.
- Vaccinations - The annual influenza vaccine and the pneumococcal vaccine markedly lower the risk of secondary bacterial bronchitis.
- Targeted supplements - Vitamin C (500‑1000mg/day), zinc (15‑30mg/day), and N‑acetylcysteine (600mg twice daily) have shown modest reductions in symptom duration.
- Avoid irritants - Stay away from second‑hand smoke, harsh cleaning chemicals, and heavy‑particle environments until symptoms subside.
- Doctor‑prescribed meds - If a bacterial infection is confirmed, a short course of antibiotics (e.g., amoxicillin) may be needed. Bronchodilators help relieve airway narrowing in chronic cases.
Each step works hand‑in‑hand with the immune system: rest conserves energy, hydration powers mucus transport, and supplements replenish nutrients that immune cells need to function optimally.

When to Seek Medical Attention
Most acute bronchitis cases resolve on their own, but certain red flags warrant a prompt doctor visit:
- Fever above 101°F (38.3°C) lasting more than three days.
- Shortness of breath or chest pain that worsens.
- Colored sputum (green, yellow, or blood‑tinged) persisting beyond a week.
- Underlying conditions such as COPD, asthma, or a weakened immune system.
- Symptoms that exceed three weeks without improvement.
Early medical intervention can prevent complications like pneumonia or a chronic worsening of bronchial damage.
Long‑Term Strategies for a Stronger Respiratory Immune Defense
Even after you’ve cleared a bout of bronchitis, the work isn’t over. Building lasting immunity involves consistent habits:
- Quit smoking-use nicotine replacement or counseling programs.
- Exercise regularly-moderate aerobic activity (e.g., brisk walking 30minutes a day) boosts lung capacity and immune surveillance.
- Maintain a balanced diet rich in fruits, vegetables, lean protein, and omega‑3 fatty acids to supply antioxidants and essential fatty acids.
- Monitor indoor air quality-use HEPA filters and keep humidity between 40‑60% to limit mold growth.
- Schedule annual health check‑ups, especially if you have chronic lung conditions.
These steps keep the airway lining healthy, ensure immune cells can reach the lungs efficiently, and reduce the frequency of future bronchitis episodes.
Frequently Asked Questions
Can antibiotics cure a cough caused by bronchitis?
Only if the cough is due to a bacterial infection. Most acute bronchitis cases are viral, so antibiotics offer no benefit and can contribute to resistance.
Is chronic bronchitis reversible?
The airway damage in chronic bronchitis is generally permanent, but symptoms can be greatly reduced by quitting smoking, pulmonary rehab, and proper medication.
How long does acute bronchitis usually last?
Most people feel better within 7‑10 days, although a lingering cough can stretch to three weeks.
Do vaccines protect against bronchitis?
Vaccines don’t prevent bronchitis directly, but they stop influenza and pneumococcal infections that often lead to secondary bronchial inflammation.
Are natural remedies like honey or ginger effective?
Honey can soothe the throat and may slightly reduce nighttime coughing. Ginger has anti‑inflammatory properties, but neither replaces medical treatment if symptoms are severe.



16 Comments
Teknolgy .com October 8, 2025 AT 19:28
Another boring health article, 🙄.
Caroline Johnson October 8, 2025 AT 22:15
Wow, this piece tries to cram every possible fact about bronchitis into one post, and it ends up sounding like a textbook, but with none of the excitement. The way it drags through cytokine pathways is exhausting, and honestly, who needs that much detail when you just want to know how to feel better?! Also, the tips about hydration and rest are good, but the article forgets to mention that over‑the‑counter cough suppressants can sometimes do more harm than good, especially if you have an underlying infection. Overall, the writing is decent, but the sheer volume of info makes it overwhelming for a casual reader. Maybe a shorter version would help, you know?
Megan Lallier-Barron October 9, 2025 AT 01:01
Funny how you can turn a medical explanation into a philosophical treatise, 😏. It makes you wonder whether the immune system is just a metaphor for our own internal struggles, constantly battling the smoke of our bad habits. If we see the lungs as a battlefield, then maybe the true victory is learning to lay down arms – quit smoking, breathe cleaner air, and let the body heal itself. In that sense, the article is a reminder that we’re not just passive victims, but active participants in our health destiny. Still, the simulator could use a bit more interactivity, like showing how stress actually spikes cortisol levels.
Val Vaden October 9, 2025 AT 03:48
Seriously, the over‑emphasis on vitamins feels like a sales pitch – 🤔. While vitamin C and zinc can help, they’re not magic bullets, and the article missed the chance to warn about over‑supplementation. Also, steam inhalation is great, but people need to be careful not to burn themselves. Bottom line: focus on basics – quit smoking, stay hydrated, and get enough rest.
lalitha vadlamani October 9, 2025 AT 06:35
It is absolutely reprehensible how modern media continues to trivialize the gravitas of chronic respiratory ailments, presenting them as mere inconveniences. One must recognize that the insidious progression of chronic bronchitis represents a profound moral failing on the part of societies that permit rampant pollution. The article, while informative, blissfully omits any condemnation of governmental inaction. Moreover, the recommendations appear superficial, lacking the stern admonition that citizens ought to demand stricter air quality legislations. In essence, the piece underestimates the ethical urgency required to combat this scourge.
kirk lapan October 9, 2025 AT 09:21
First of all, let me just say that the entire "immune response" section reads like a college lecture written by a bored professor who never left his 1990s lab coat on. The article throws around terms like IL‑6 and TNF‑α as if they were the latest TikTok trends, but forgets to explain why a layperson should care about those cytokines at all. It’s also weird that they talk about "macrophage over‑activation" without mentioning that smoking literally clouds the whole alveolar environment, making those cells wander around like lost tourists. And don’t get me started on the "supplements" list – they suggest 1000 mg of vitamin C a day, which is basically a nonsense number that will just make you dump it in the toilet. If you actually wanted to help someone, you’d advise them to quit smoking, get a proper diagnosis, and maybe see a pulmonologist instead of handing them a grocery‑store supplement flyer.
that probably won’t work on any browser older than 2020. The whole thing feels like a rushed attempt to cram SEO keywords rather than a genuine effort to educate. If you’re looking for a deep dive, you’ll need to go to a peer‑reviewed journal, not this glossy web page that seems to think “steam inhalation” is a groundbreaking discovery. Last but not least, the article repeats the same bullet points in the “Key Takeaways” that were already covered in the intro – a classic case of lazy copy‑pasting. In short, it’s a mix of half‑baked science, marketing fluff, and a UI that looks like it was assembled by a toddler with a cut‑and‑paste habit.
Also the formatting is all over the place – there’s a random tag that never closes, and the simulator button is hidden behind a
Landmark Apostolic Church October 9, 2025 AT 12:08
Reading through that detailed breakdown makes me appreciate how our bodies are basically tiny ecosystems fighting for balance. The way macrophages and neutrophils coordinate reminds me of a well‑orchestrated jazz ensemble, each instrument playing its part. Still, the article could've highlighted how regular walks in nature boost immune surveillance – literally letting fresh air do its job. Anyway, solid info for anyone wanting to understand the battle happening in their lungs.
Matthew Moss October 9, 2025 AT 14:55
One must, with the greatest sincerity, affirm that the discourse presented above is utterly lacking in patriotic spirit. Our great nation has always stood against the scourge of disease, and it is incumbent upon each citizen to support public health measures, not to indulge in personal whims like smoking. Therefore, I implore all readers to embrace the virtues of discipline and temperance for the betterment of our collective wellbeing.
Antonio Estrada October 9, 2025 AT 17:41
I agree with the previous comment about regular exercise – even a modest daily walk can enhance mucociliary clearance and support immune cell circulation. Combining that with a balanced diet provides the necessary micronutrients for optimal immune function. It’s a holistic approach that respects both the body’s needs and scientific evidence.
Jarrod Benson October 9, 2025 AT 20:28
Yo, this article really nails the basics but also goes deep enough to keep the science geeks happy. I love how they broke down the difference between acute and chronic bronchitis – makes it clear why you can’t just “wait it out” when you’ve been smoking for years. The lifestyle tips are solid, especially the part about staying hydrated; I swear a big glass of water can thin that nasty mucus in minutes. Also, the bit about vaccines is spot‑on – most people don’t realize that preventing flu can stop a whole chain reaction leading to bronchial infection. If you’re still on the fence about quitting smoking, think of your lungs as a garden: you gotta pull out the weeds before they choke the flowers.
Liz . October 9, 2025 AT 23:15
Totally agree, staying hydrated is key – I always keep a water bottle at my desk.
tom tatomi October 10, 2025 AT 02:01
Honestly, all this hype about immune cells is just a distraction from the fact that most people won’t change their habits no matter how many tables you show them.
Tom Haymes October 10, 2025 AT 04:48
You’re right that habits are tough, but small steps like adding a daily walk can add up. Keep encouraging each other, and the change becomes less intimidating.
Ajayi samson October 10, 2025 AT 07:35
What a waste of time – this piece tries to sound scientific but ends up being a shallow PR stunt for the health industry. People need real solutions, not a list of “drink water and quit smoking” clichés.
Lief Larson October 10, 2025 AT 10:21
Interesting read, especially the part about how pollution impacts lung health. It’s vital we talk about these issues more often.
Julia Grace October 10, 2025 AT 13:08
Glad you found the pollution bit useful! Just a heads‑up – you might also want to check out local air quality apps – they can give you real‑time data so you can plan outdoor activities when the air is cleaner.
Write a comment