Most people hear "COPD" and think of one thing: trouble breathing. But behind that single label are two very different diseases-chronic bronchitis and emphysema. They’re not just two sides of the same coin. They’re two different machines breaking down in the same car, and knowing which one is failing changes everything about how you fix it.
What Exactly Is COPD?
COPD stands for Chronic Obstructive Pulmonary Disease. It’s not a single illness. It’s a group of lung conditions that make it hard to breathe out. About 380 million people worldwide have it. In the U.S. alone, 16 million are diagnosed, and many more don’t know they have it. For decades, doctors treated it like one disease. But now we know better. The two main players are chronic bronchitis and emphysema-and they damage your lungs in completely different ways.
Chronic Bronchitis: The Mucus Problem
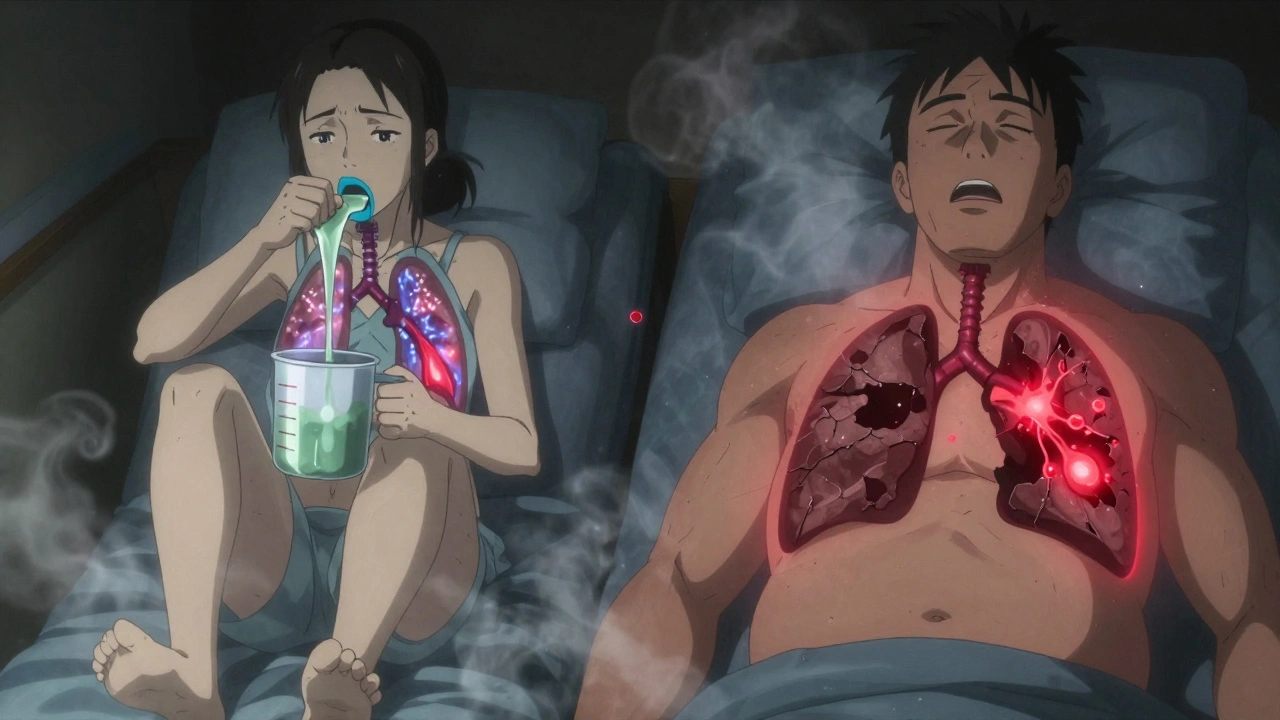
If you’ve got chronic bronchitis, your airways are flooded. Not with water, but with mucus. The lining of your bronchial tubes gets inflamed and swollen. Goblet cells-tiny mucus factories-multiply like crazy. Instead of producing 10 to 100 milliliters of mucus a day like a healthy lung, your lungs are making 100 to 200 mL. That’s almost a cup of thick gunk daily.
The result? A cough that won’t quit. Not just a little cough. A productive cough-meaning you’re bringing up phlegm-for at least three months a year, for two years straight. That’s the official definition. Most people with this condition cough first thing in the morning, sometimes clearing out 30 to 100 mL of mucus. One patient on Reddit measured it: 100 mL every morning for eight years, using a measuring cup.
This isn’t just annoying. That mucus clogs your airways. It traps bacteria. That’s why people with chronic bronchitis get infections so easily-especially in winter. Their lungs are basically a breeding ground. And because the tiny hair-like structures called cilia that normally sweep mucus out are damaged, the gunk just sits there.
Doctors call this the "blue bloater" phenotype. Why? Because low oxygen levels turn lips and fingernails blue (cyanosis), and fluid builds up in the legs from heart strain. Their oxygen saturation often dips to 85-89%. They’re tired, swollen, and winded-even walking short distances.
Emphysema: The Air Sac Collapse
Emphysema is the opposite problem. No extra mucus. No constant cough. Instead, the air sacs in your lungs-the alveoli-start to die. These are the tiny balloons where oxygen enters your blood and carbon dioxide leaves. In emphysema, the walls between them break down. They merge into big, useless air pockets. You lose 30-50% of your lung’s natural springiness. It’s like losing the elastic in your socks.
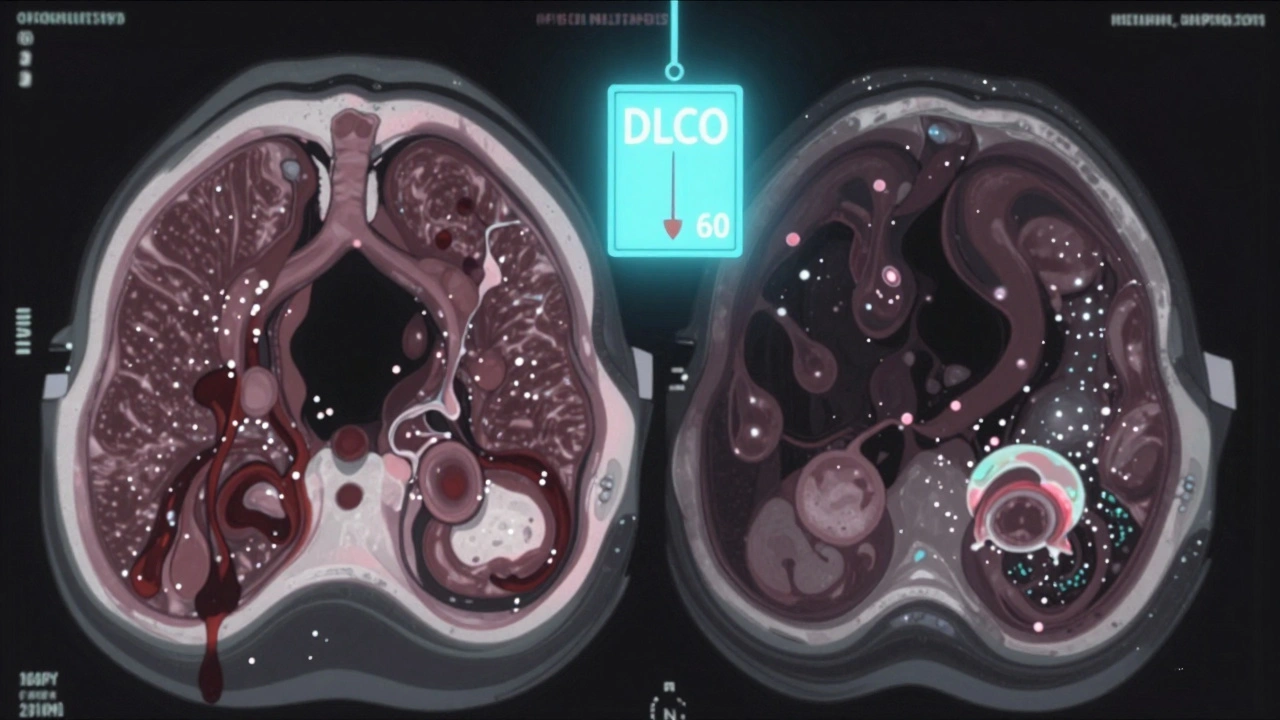
This isn’t just about airflow. It’s about gas exchange. Your lungs can’t pull oxygen in efficiently. Diffusing capacity for carbon monoxide (DLCO)-a key test-drops below 60% of normal. In advanced cases, it’s half that. You’re breathing hard, but your blood isn’t getting enough oxygen.
The main symptom? Progressive breathlessness. At first, it’s only when you climb stairs. Then it’s walking on flat ground. Eventually, you can’t speak more than five or six words without stopping to catch your breath. That’s the hallmark of emphysema. No cough? No mucus? That’s normal. Many emphysema patients never cough at all.
They’re the "pink puffers." Why? Because they’re hyperventilating-breathing fast and shallow-to keep oxygen up. Their skin stays pink. But their chest becomes barrel-shaped. Their lungs are overinflated, stuck open like a balloon that won’t deflate. Their residual volume (air left after exhaling) can exceed 150% of normal.
How Do Doctors Tell Them Apart?
You can’t tell just by listening to a cough. You need tests.
- Pulmonary Function Tests (PFTs): Both show low FEV1/FVC ratio (less than 70%), meaning airway blockage. But emphysema has a low DLCO. Chronic bronchitis? DLCO is usually normal or only slightly down.
- CT Scans: Emphysema shows dark, low-density areas in the lungs-holes where tissue used to be. Chronic bronchitis shows thickened airway walls, especially on expiratory scans.
- 6-Minute Walk Test: Emphysema patients drop oxygen fast-below 88% within two minutes. Chronic bronchitis patients stay oxygenated but stop because they’re too out of breath.
- Physical Signs: Barrel chest? Likely emphysema. Swollen ankles and blue lips? Likely chronic bronchitis.
And here’s the kicker: 85% of people with severe COPD have both. But one usually dominates. That’s what matters for treatment.
Treatment Isn’t One-Size-Fits-All
For years, everyone got the same inhalers. Now we know that’s a mistake.
Chronic bronchitis patients need help clearing mucus. Mucolytics like carbocisteine reduce flare-ups by 22%. Hypertonic saline nebulizers thin the gunk-73% of users report better clearance. Roflumilast, a pill taken daily, cuts exacerbations by 17.3%. But here’s the danger: inhaled steroids? They increase pneumonia risk by 40% in these patients. So doctors avoid them unless absolutely necessary.
Emphysema patients need to reduce trapped air. Lung volume reduction surgery (LVRS) works for some-35% better outcomes than standard care. Endobronchial valves (tiny one-way devices placed via bronchoscopy) help 65% of eligible patients. They let air out but not in, collapsing the worst-damaged parts of the lung. In the IMPACT trial, patients walked 35% farther after placement.
For those with genetic emphysema (1-2% of cases), alpha-1 antitrypsin deficiency, weekly infusions of the missing protein can slow decline. The FDA just approved an inhaled version in 2023-20% improvement in lung function after a year.
Why This Matters for Daily Life
It’s not just about meds. It’s about your life.
Chronic bronchitis patients spend hours every day doing chest physiotherapy. Some use a device that vibrates mucus loose. Others wear oxygen tanks all day. One woman in Oregon told her doctor she couldn’t hug her grandchildren without stopping to cough.
Emphysema patients live with constant air hunger. They avoid crowds, restaurants, even car rides because talking is exhausting. Portable oxygen concentrators help-but they’re heavy. One man said he stopped going to his grandson’s baseball games because walking to the bleachers made him feel like he was drowning.
Both groups struggle with adherence. Sixty-eight percent of chronic bronchitis patients can’t keep up with 4-6 daily inhalers. Fifty-two percent of emphysema patients say oxygen limits their freedom.
But when treatment is targeted? Outcomes improve. A 2022 study showed patients getting the right therapy for their type had 27% fewer hospital stays. That’s not just a number. That’s fewer ER visits. Fewer nights in the hospital. More time at home.

What’s Changing in 2025?
The field is moving fast.
- A new acoustic device, launched in Europe in 2024, uses sound waves to shake mucus loose in chronic bronchitis-reducing flare-ups by 32%.
- The NIH is tracking 10,000 patients through the SPIROMICS-2 study, looking for blood markers that predict who’ll respond to new biologic drugs.
- Bronchoscopic thermal vapor ablation, a minimally invasive procedure for emphysema, shows 78% success at two years.
- Drugmakers are developing new mucoregulators that target TMEM16A channels-key players in mucus overproduction.
And regulators are catching up. The FDA now requires all new COPD trials to split results by phenotype. That’s huge. It means future drugs will be designed for specific types of COPD-not a one-size-fits-all approach.
What Should You Do?
If you or someone you love has COPD, ask your doctor:
- "Do I have more bronchitis or emphysema?"
- "What’s my DLCO? Is it below 60%?"
- "Have I had a CT scan to check for air sac damage?"
- "Am I on the right meds for my type?"
- "Could I benefit from lung volume reduction or a mucus-clearing device?"
Don’t accept "it’s just COPD" as an answer. That’s like saying "it’s just a car problem" when the engine’s blown versus the brakes are worn. The fix is totally different.
Join a support group. The COPD Foundation has over 200 local chapters. People who stick with them report better self-management after six months. You’re not alone. And better treatments are coming.
Can you have chronic bronchitis without emphysema?
Yes, but it’s rare. Most people with long-term COPD have some features of both. However, chronic bronchitis can exist on its own, especially in long-term smokers who haven’t developed significant alveolar destruction. The key is whether the main problem is mucus overproduction and airway inflammation (bronchitis) versus destroyed air sacs and loss of elasticity (emphysema). Pulmonary function tests and CT scans can tell the difference.
Is emphysema worse than chronic bronchitis?
Neither is "worse"-they’re just different. Emphysema often leads to severe oxygen problems and early activity limits. Chronic bronchitis brings frequent infections, hospitalizations, and mucus-related exhaustion. Emphysema patients may live longer without hospital visits, but their breathing gets worse faster. Chronic bronchitis patients may have better oxygen levels but suffer more from daily symptoms and flare-ups. The real danger is when neither is properly identified and treated.
Can quitting smoking reverse COPD?
No, it can’t reverse damage already done. But quitting is the single most effective thing you can do. It slows progression by up to 50%. Your lungs stop getting worse faster. Inflammation drops. Cilia begin to recover. Mucus production decreases. Your risk of infections and hospital stays drops sharply. Even if you’ve smoked for 40 years, quitting at 60 still adds years to your life.
Do inhalers work the same for both conditions?
Not exactly. Both benefit from LAMA/LABA combinations (long-acting bronchodilators), which open airways. But chronic bronchitis patients need mucolytics and sometimes roflumilast to reduce mucus and flare-ups. Emphysema patients don’t benefit from these. In fact, inhaled steroids-which some use for inflammation-can increase pneumonia risk in bronchitis patients by 40%. The right combo depends on your phenotype.
What’s the life expectancy with COPD?
It varies widely. With early diagnosis and proper management, many live 10-20 years or more after diagnosis. Emphysema patients with severe disease and low DLCO have higher mortality, especially if they continue smoking. Chronic bronchitis patients with frequent exacerbations have higher hospitalization rates, which also shorten life. But quitting smoking, using the right medications, getting pulmonary rehab, and avoiding infections can dramatically improve both quality and length of life.
Final Thought
COPD isn’t one disease. It’s two. And treating them the same is like giving the same medicine for a broken leg and a bad heart. The future of COPD care isn’t about more inhalers. It’s about precision-knowing which part of your lungs is failing, and fixing that part specifically. If you’ve been told you have COPD, ask for the details. Your next breath depends on it.


13 Comments
Tiffany Sowby December 10, 2025 AT 04:47
This post is just a long-winded ad for Big Pharma. Everyone knows smoking kills your lungs - no need to turn it into a medical textbook. I’ve got COPD and I just use my inhaler and ignore all this jargon.
Asset Finance Komrade December 10, 2025 AT 22:26
One must consider the ontological implications of pulmonary dysfunction within the capitalist framework of healthcare commodification. The binary distinction between bronchitis and emphysema is a linguistic construct imposed by Western medicine to maintain epistemic hegemony. 🤔
Brianna Black December 11, 2025 AT 22:18
OMG I just read this and I’m crying 😭 My mom had COPD for 12 years and no one ever told us the difference between bronchitis and emphysema - she was just given a neb and told to "breathe better." This is the most important thing I’ve read all year. Thank you for writing this with so much heart and science. I’m sharing this with every doctor I know.
Stacy Tolbert December 13, 2025 AT 00:00
I’ve been living with chronic bronchitis for 8 years. Every morning I cough up enough mucus to fill a coffee mug. I used to think I was just a "bad smoker," but now I realize my lungs are just factories gone rogue. Carbocisteine changed my life - no more 3 a.m. coughing fits. If you’re still on steroids for this? Stop. They’re making it worse.
Ronald Ezamaru December 13, 2025 AT 21:47
Great breakdown. I’m a respiratory therapist and this is exactly what we teach new grads. The "blue bloater" vs "pink puffer" labels are outdated but still useful for quick clinical triage. The real win is recognizing that 85% have both - so treatment should be layered, not one-size-fits-all. Also, pulmonary rehab works. Like, 70% improvement in six weeks. People don’t know that.
Ryan Brady December 15, 2025 AT 12:03
Why are we even talking about this? The government’s gonna make you wear oxygen masks in public next. My cousin got diagnosed and now he’s got a machine strapped to his back like a robot. This is what happens when you let the medical industrial complex take over. Just quit smoking and stop complaining.
Raja Herbal December 15, 2025 AT 20:46
So... you’re telling me after 30 years of smoking, I’m not just "a smoker" - I’m a "blue bloater"? And now I need a fancy nebulizer and a pill that costs $800/month? Good luck with that, buddy. In India, we just drink ginger tea and pray. 😅
Iris Carmen December 17, 2025 AT 12:48
idk if this is real or just someone trying to sound smart but i think i have emphysema bc i get outta breath just walking to my mailbox and i dont even cough. also i hate oxygen tanks they look like sci fi gear
Rich Paul December 18, 2025 AT 02:24
DLCO is the key metric bro. If it’s below 60%, you’re in the emphysema zone. FEV1/FVC just tells you there’s obstruction, but DLCO tells you if the alveoli are toast. Also, if your CT shows honeycombing or low attenuation areas? That’s not inflammation - that’s tissue death. You can’t un-destroy alveoli. Stop hoping for a miracle and start prepping for LVRS or valves. I’ve seen 12 patients get endobronchial valves - 8 of them walked 2x farther after. It’s not magic, it’s physics.
Delaine Kiara December 19, 2025 AT 20:55
Let me tell you something - I used to be a nurse in a pulmonary unit. I’ve seen people with chronic bronchitis cough so hard they vomit blood. I’ve seen emphysema patients with barrel chests so extreme they can’t fit into wheelchairs. And I’ve seen doctors give them the same inhalers and say "it’s all COPD." That’s not medicine - that’s laziness. The fact that the FDA now requires phenotype-split data? That’s a win. But it took 40 years. We need to stop calling it "COPD" altogether. It’s like calling diabetes "high sugar" and not distinguishing between Type 1 and Type 2. We’re still in the dark ages.
And don’t even get me started on the people who say "just quit smoking." I had a patient who quit at 55 after 50 years. He still had emphysema. His lungs were ruined. But he lived 10 more years without a single hospital stay. That’s the power of quitting - not reversal, but stopping the bleeding.
Also, the new inhaled alpha-1 therapy? Game changer. My cousin has the deficiency. He got it last year. His DLCO went from 38% to 51%. He’s hiking again. I cried when he told me. This isn’t just science - it’s hope.
Ruth Witte December 20, 2025 AT 02:56
YOU ARE NOT ALONE 💪💖 I had chronic bronchitis and thought I was broken - but now I do my mucus-clearing device every morning and I hug my grandkids again! 🤗💕 It’s hard, but you can still live FULLY. Get a support group. Try the new sound wave device - it’s like a magic wand for your lungs! 🌟 You got this!
Noah Raines December 21, 2025 AT 17:01
My dad’s got emphysema. He’s 72. Used to golf every weekend. Now he can’t walk to the garage without stopping. We got him the endobronchial valves last year. He’s walking to the mailbox now. Not golfing, but he’s not sitting in a chair all day either. It’s not perfect, but it’s progress. The thing no one talks about? The mental toll. You don’t just lose lung function - you lose your old self. This post gets that.
Katherine Rodgers December 23, 2025 AT 05:05
So let me get this straight - after spending 20 years smoking, now you want me to pay $10k for a valve I don’t even know if I qualify for? And the government’s gonna make drug trials split by phenotype? Cool. So now instead of one drug for everyone, we get 5 different drugs for 5 different ways to die from cigarettes? Thanks, capitalism. At least the blue bloaters can still cough loudly enough to wake the neighbors.