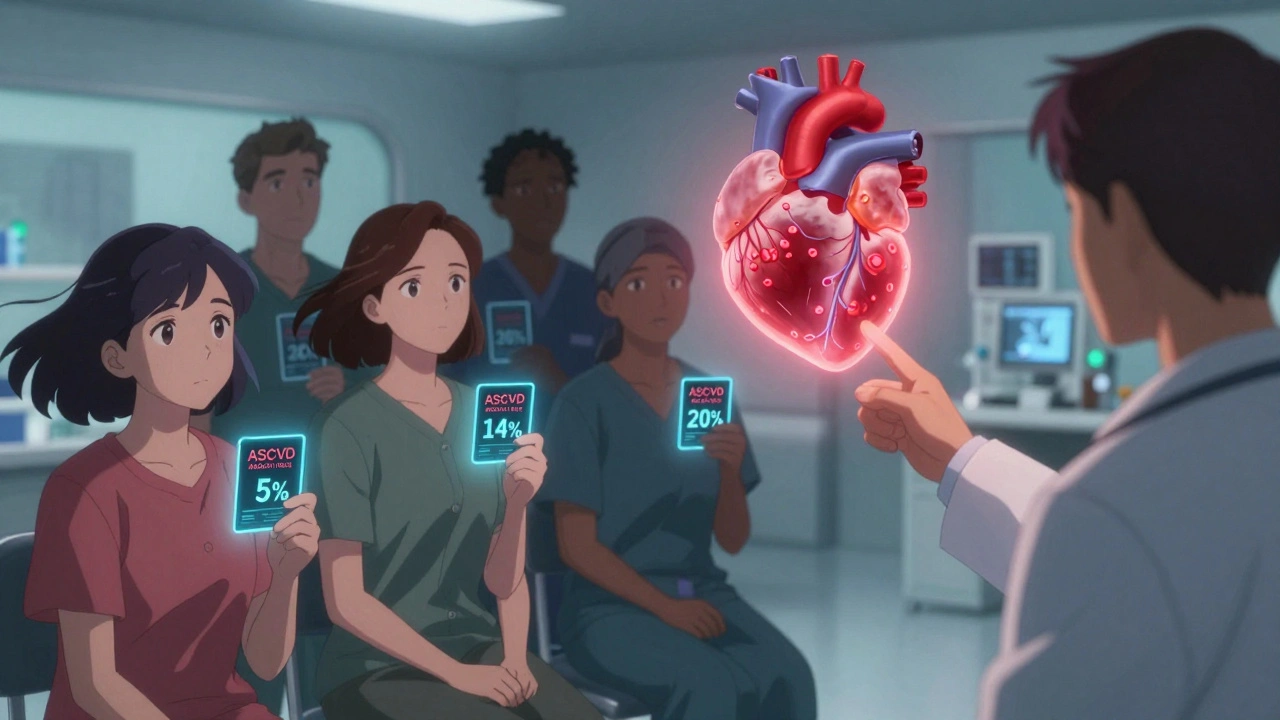
When we talk about heart disease risk, the likelihood of developing conditions like coronary artery disease, heart attack, or stroke due to biological and behavioral factors. Also known as cardiovascular disease risk, it’s not just about age or family history—it’s shaped by what you take, what you eat, and how your body responds to stress. Many people think high cholesterol is the main driver, but that’s only part of the story. The real picture includes how medications interact, whether your blood pressure is quietly creeping up, and if you’re taking drugs that might be harming your heart instead of helping it.
Hypertension medications, drugs used to lower blood pressure like ACE inhibitors, beta-blockers, or diuretics can be lifesavers—but they don’t work in isolation. Mixing them with common OTC painkillers like ibuprofen can spike your blood pressure or damage your kidneys. Even something as simple as too much salt or alcohol can undo their effects. Then there’s statin interactions, how cholesterol-lowering drugs like atorvastatin or simvastatin behave when taken with other meds, especially HIV treatments or antibiotics. Some combinations raise the risk of muscle damage or liver stress, which can silently worsen heart health. And if you’ve had a stent, dual antiplatelet therapy, the combo of aspirin and clopidogrel used to prevent clots after heart procedures reduces heart attacks but increases bleeding risk—so getting the duration right matters just as much as taking the pills.
It’s not just about popping pills. Stress tests and ECGs catch problems early, but they won’t fix what’s happening in your arteries because of poor sleep, chronic inflammation, or supplements like garlic that thin your blood too much. The most effective way to lower heart disease risk isn’t a miracle drug—it’s understanding how everything connects: your meds, your diet, your other conditions, and even how you manage daily stress. Below, you’ll find clear, no-fluff guides on exactly what to watch for, what to ask your doctor, and what steps actually move the needle—whether you’re managing high blood pressure, taking statins, recovering from a stent, or just trying to keep your heart healthy without relying on guesswork.