What Is an ASCVD Risk Calculator?
Every year, over 800,000 Americans have a heart attack or stroke. Many of these events happen to people who had no symptoms and thought they were fine. That’s where the ASCVD risk calculator comes in. It doesn’t predict the future-it gives you a realistic snapshot of your chances of having a heart attack or stroke in the next 10 years based on simple, measurable facts about your health.
The ASCVD Risk Estimator, developed by the American College of Cardiology and the American Heart Association in 2013 and updated in 2018, uses data from decades of research across tens of thousands of people. It’s not a guess. It’s math built on real studies like the Framingham Heart Study and the Atherosclerosis Risk in Communities Study. The tool looks at nine things: your age, sex, race, total cholesterol, HDL (good) cholesterol, systolic blood pressure, whether you’re on blood pressure meds, if you have diabetes, and if you smoke. Plug those in, and it spits out a percentage.
That number isn’t just for doctors. It’s meant to start a conversation. A 12% risk means you have a 1 in 8 chance of having a major heart event before you turn 70. That’s serious. But it’s also actionable.
How the ASCVD Score Breaks Down Risk Levels
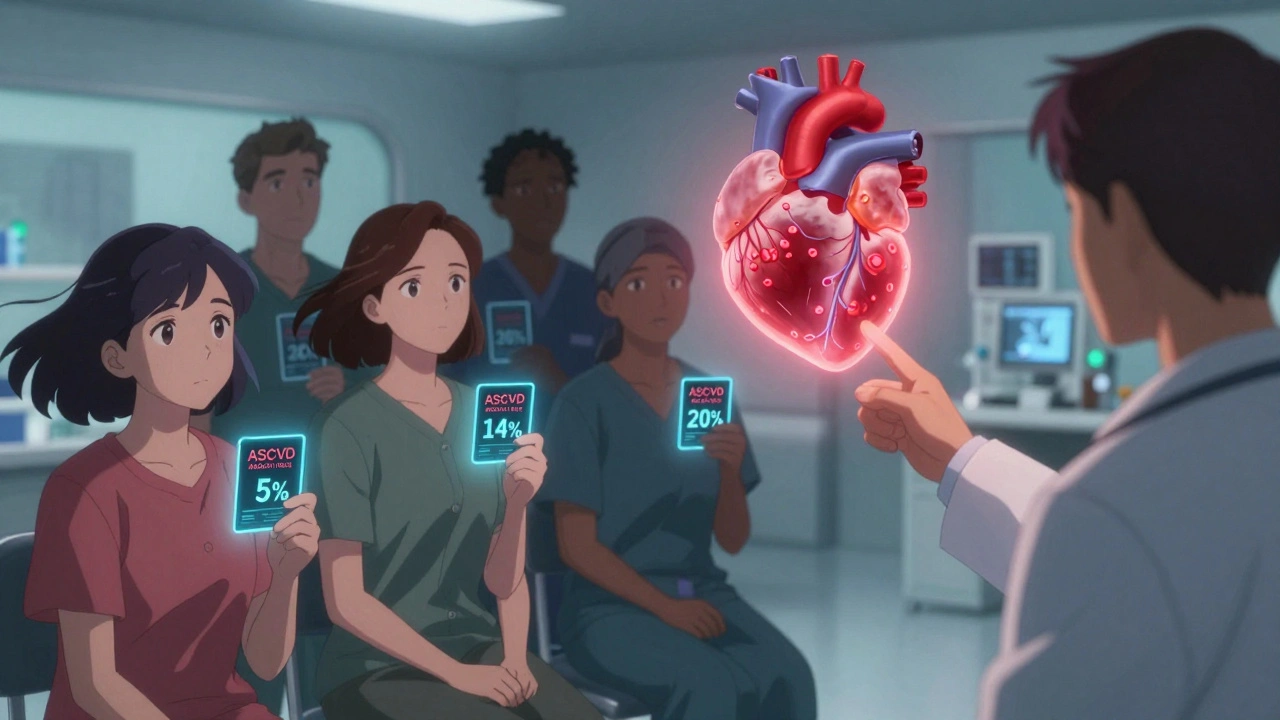
The calculator doesn’t just give you a number-it puts it into categories that guide what happens next:
- Low risk: Under 5% - Your heart is in good shape. Focus on staying healthy.
- Borderline risk: 5% to 7.4% - Time to pay attention. Small changes can make a big difference.
- Intermediate risk: 7.5% to 19.9% - This is the gray zone. Many people land here. That’s when things get interesting.
- High risk: 20% or higher - You’re in the danger zone. Medication is often needed.
Most people who get screened fall into the intermediate range. That’s not an accident. It’s by design. The goal isn’t to label everyone as high or low. It’s to find the people who need more than just a pep talk.
For example, a 52-year-old woman with high blood pressure, borderline cholesterol, and a history of smoking might have a 14% 10-year risk. That’s not “maybe someday.” That’s “you need to act now.”
Why the ASCVD Calculator Isn’t Perfect-And What to Do About It
Here’s the hard truth: the ASCVD calculator was built mostly on data from White and Black Americans. It doesn’t work as well for everyone. Studies show it underestimates risk by 15% to 25% for American Indians, South Asian Americans, and Puerto Ricans. For East Asian Americans and Mexican Americans, it sometimes overestimates risk by 10% to 20%.
That doesn’t mean you throw it out. It means you use it smarter.
Doctors who rely only on the ASCVD score are missing half the picture. That’s why experts like Dr. Donald Lloyd-Jones say it’s a conversation starter, not a final answer. If your score says you’re borderline but you’re a South Asian man with a family history of early heart disease, your real risk is probably higher. Same if you live in a neighborhood with no grocery stores, work two jobs, and sleep less than six hours a night. Those things matter.
The 2023 AHA Presidential Advisory called this out directly: the current tool underestimates risk for 28 million Americans because of racial and ethnic gaps in the original data. That’s why new versions are being tested-with machine learning models trained on more diverse populations. One early version improved accuracy for South Asian Americans by 18%.
What Comes After the Score? CAC, hsCRP, and Other Tools
If your ASCVD score puts you in the intermediate zone (7.5%-19.9%), you’re not stuck. There’s a next step.
The most powerful tool for refining risk is the coronary artery calcium (CAC) scan. It’s a quick, non-invasive CT scan that shows actual calcium buildup in your heart arteries. No dye. No needles. Just a few seconds in the machine.
Here’s what happens when you add it in: 52% of intermediate-risk patients get reclassified. Some drop to low risk. Others jump to high risk. That changes everything. A CAC score of zero means your risk is lower than the calculator says. A score over 100? You’re likely in the high-risk group, even if your numbers look okay.
Other tools help too:
- hsCRP measures inflammation. High levels mean your arteries are under stress, even if cholesterol looks fine.
- Ankle-brachial index (ABI) checks for blocked arteries in your legs-a sign your heart arteries might be blocked too.
- Lipoprotein(a) is a genetic risk factor. If your family has early heart disease, this test might be worth asking for.
One study found that adding CAC scoring changed treatment plans in 68% of intermediate-risk patients. That’s not a minor tweak. That’s a full course correction.

When to Start Thinking About Lifetime Risk
Most people think in terms of the next 10 years. But heart disease doesn’t wait. A 45-year-old with a 6% 10-year risk might feel safe. But if they’ve got high blood pressure, high cholesterol, and smoke, their lifetime risk could be over 50%.
That’s why the guidelines now say: if you’re under 55 and your 10-year risk is borderline or intermediate, look at your lifetime risk. About 78% of heart attacks and strokes happen in people whose 10-year risk is under 20%. That’s the silent majority.
Think of it like this: if you’re 48 and your 10-year risk is 8%, you might not need a statin today. But if your lifetime risk is 60%, you need to act now to change your trajectory. Lifestyle changes-diet, movement, sleep, stress management-have the biggest impact over time.
How Clinicians Actually Use the Calculator (And Where They Go Wrong)
In theory, the ASCVD calculator is simple. In practice? It’s messy.
Doctors use it in 92% of major electronic health systems like Epic and Cerner. Over 15 million calculations are done every year in the U.S. That’s good. But here’s the problem:
- 22% of patients misreport whether they smoke. One person says “I quit 5 years ago,” but the system still marks them as a smoker.
- Blood pressure readings vary by 8-12 mm Hg depending on how it’s taken. If you’re checked right after coffee or while stressed, your number is inflated.
- One in three primary care doctors misclassifies intermediate risk as low risk. That means people who should be getting statins or lifestyle coaching are being told to “come back in a year.”
And yet, even with these flaws, the calculator has improved care. Since 2014, appropriate statin use has gone up 27%. But only 58% of people who should be on statins actually are. That’s a gap. And it’s not because doctors don’t know. It’s because the system is broken.
The real power of the calculator isn’t in the number. It’s in the conversation it forces. “Your risk is 15%. That’s higher than 85% of people your age. What are you willing to change?” That question changes outcomes.
The Future: Genes, Social Factors, and Personalized Risk
The next generation of risk tools is already here. The American Heart Association’s PREVENT Online Calculator, launched in January 2023, goes beyond cholesterol and blood pressure. It includes social factors:
- Neighborhood deprivation index (how safe, walkable, and resourced your area is)
- Food insecurity (how often you have to choose between medicine and groceries)
- Education level and income
Why? Because living in a food desert or working three shifts a week raises your heart risk as much as smoking. A 2021 study in Circulation found these factors predict 23% higher cardiovascular death-on top of all the usual risks.
And then there’s genetics. The UK Biobank study showed that adding a polygenic risk score (based on 6.6 million genetic markers) improved prediction accuracy by 14.3% in intermediate-risk patients. That’s huge. Imagine knowing your genetic risk at 30, not 55.
This isn’t science fiction. It’s happening. The future of heart risk isn’t just a calculator. It’s a digital twin of your health-clinical data, lifestyle, environment, and genes-all woven together.
What You Should Do Right Now
If you’re between 40 and 79, ask your doctor for your ASCVD score. Don’t wait for them to bring it up. Bring it up yourself.
Here’s how:
- Get your latest cholesterol panel (total, HDL, LDL).
- Know your blood pressure numbers. Take them at home, not just at the clinic.
- Be honest about smoking-even if you quit, say so.
- Ask: “What’s my 10-year ASCVD risk? What’s my lifetime risk?”
- If you’re in the intermediate range, ask: “Should I get a CAC scan?”
- If you’re under 55, ask: “Is my lifetime risk high?”
Don’t let a number scare you. Let it empower you. A 15% risk isn’t a death sentence. It’s a warning light. And warning lights exist so you can fix the problem before it breaks down.
What About the Reynolds or MESA Scores?
You might hear about other calculators. The Reynolds Risk Score adds hsCRP and family history. The MESA score uses CAC data to give you a “coronary age”-like saying your heart is 78 even though you’re 55.
They’re great tools. But they’re not the standard. The ASCVD calculator is the one integrated into guidelines, insurance systems, and EHRs. If you’re going to use one tool, use this one. Then, if needed, layer on the others.
Think of the ASCVD score as your baseline. Everything else is an upgrade.
Final Thought: Risk Is Not Destiny
The ASCVD calculator doesn’t tell you what will happen. It tells you what’s likely if nothing changes. That’s the key.
Change your diet. Walk 30 minutes a day. Quit smoking. Sleep better. Take your meds. Those things don’t just lower your score. They change your life.
Heart disease isn’t random. It’s preventable. The calculator just helps you see the path.


15 Comments
Ali Bradshaw December 4, 2025 AT 23:46
I've been using this calculator for my patients for years. It's not perfect, but it gets the conversation started. Most people don't realize how much lifestyle matters until they see the number. One guy thought he was fine until his score came back at 18%. Now he walks 5 miles a day and quit smoking. Small changes, huge impact.
an mo December 5, 2025 AT 23:25
The ASCVD calculator is a neoliberal tool designed to pathologize normal aging. It's not medicine-it's actuarial science disguised as healthcare. They're quantifying your mortality to sell you statins and push corporate wellness agendas. The data? Biased. The motives? Profit-driven. The outcome? Overmedication of the working class.
Lynette Myles December 7, 2025 AT 00:24
They left out diet quality. And sleep apnea. And chronic stress. And glyphosate exposure. And EMF radiation. This calculator is a joke. It's based on 1980s data from people who didn't even have smartphones. You can't reduce heart disease to cholesterol and blood pressure. That's like diagnosing cancer with a thermometer.
Annie Grajewski December 8, 2025 AT 06:40
ok but like... why do we even need this? i got my cholesterol checked last year and my doc just said 'eat less pizza' and handed me a pamphlet. also my cousin's grandpa had a heart attack at 82 and he ate bacon every day. so... what's the point? also can we talk about how the whole 'CAC scan' thing is just a fancy x-ray that costs $300 and i'm pretty sure it's just a way for radiology departments to make bank?
Jimmy Jude December 9, 2025 AT 00:12
This isn't about heart health. This is about control. They want you to believe your body is a broken machine that needs constant monitoring, testing, and pharmaceutical fixes. But real health? It's in the soil, in the sun, in the quiet. The system doesn't want you to heal. It wants you to pay. Every scan, every pill, every 'risk score'-it's all just another hook in the machine. Wake up.
Rupa DasGupta December 9, 2025 AT 23:58
I'm from India and my doctor said my score is 14%... but my uncle died at 47 from heart attack and my mom has diabetes. So what does this number even mean? 😔 I feel like I'm being told I'm 'borderline' when I'm actually screaming inside. And no one listens. And I can't afford a CAC scan. This system is broken. 💔
Marvin Gordon December 11, 2025 AT 12:21
I love that this post highlights the CAC scan. I had mine done last year-scored zero. My ASCVD was 12%. My doctor was stunned. I didn't need a statin. I needed to stop stressing over work. That scan saved me from unnecessary meds and gave me peace. Don't skip it if you're intermediate. It's not expensive. It's not invasive. It's life-changing.
ashlie perry December 13, 2025 AT 11:43
The system is rigged. They use data from white people to judge brown people. Then they blame you for being high risk. I'm Mexican. My score says I'm over 20%. But my family eats beans, corn, and salsa. We don't eat processed junk. The calculator doesn't see that. It just sees 'Hispanic' and adds 15% because of bias. This isn't science. It's racism with a spreadsheet.
Kylee Gregory December 14, 2025 AT 23:18
I think the real value here isn't the number-it's the awareness. Before I saw my score, I thought 'I'm young, I'm fine.' But once I understood my lifetime risk was 58%, I started cooking, sleeping better, and actually listening to my body. The calculator didn't diagnose me. It awakened me. That's powerful. We need more tools like this that make the invisible visible.
Chris Brown December 15, 2025 AT 12:17
It is a moral failing when individuals refuse to take personal responsibility for their health. The data is clear. Smoking, poor diet, and inactivity are the primary drivers of cardiovascular disease. Blaming the algorithm is an abdication of agency. If you are 14% risk, you have been given a gift: the opportunity to change. Choose wisely.
Manish Shankar December 16, 2025 AT 01:38
Respected sir/madam, I must express my deep appreciation for this comprehensive exposition on ASCVD risk stratification. In the Indian context, where healthcare access remains uneven, such tools are invaluable for prioritizing interventions. However, cultural dietary patterns-such as frequent use of ghee and refined carbohydrates-require localized calibration. We must adapt global models to regional realities with humility and precision.
luke newton December 16, 2025 AT 22:47
You think this is bad? Wait until they start using AI to predict your 'moral risk score' based on your social media. Next thing you know, your insurance denies you because your 'lifestyle ethics' are too low. This is how they control us. They don't care if you live or die. They care if you pay. And if you don't? They'll just label you 'high risk' and move on.
Ada Maklagina December 17, 2025 AT 04:29
I got my score last month. 11%. My doctor said 'you're fine.' I asked about the CAC scan. He said 'not necessary.' I paid out of pocket. Score was 217. Now I'm on a statin. Don't trust your doctor's gut. Trust the scan.
Harry Nguyen December 18, 2025 AT 12:56
The American Heart Association is a puppet of Big Pharma. They invented this calculator so they could sell more statins. You know what lowers heart risk? Vitamin D. Omega-3s. Sunshine. Not pills. But you won't hear that from them because you can't patent the sun. This whole system is a scam.
sean whitfield December 20, 2025 AT 09:19
So you're telling me that if I'm a 45-year-old guy who eats kale and meditates but lives in a bad neighborhood, I'm at higher risk than a 60-year-old who smokes but has a mansion in Malibu? That's not science. That's socialism. The system should reward good choices, not punish people for being poor. This isn't health. It's class warfare with a stethoscope.