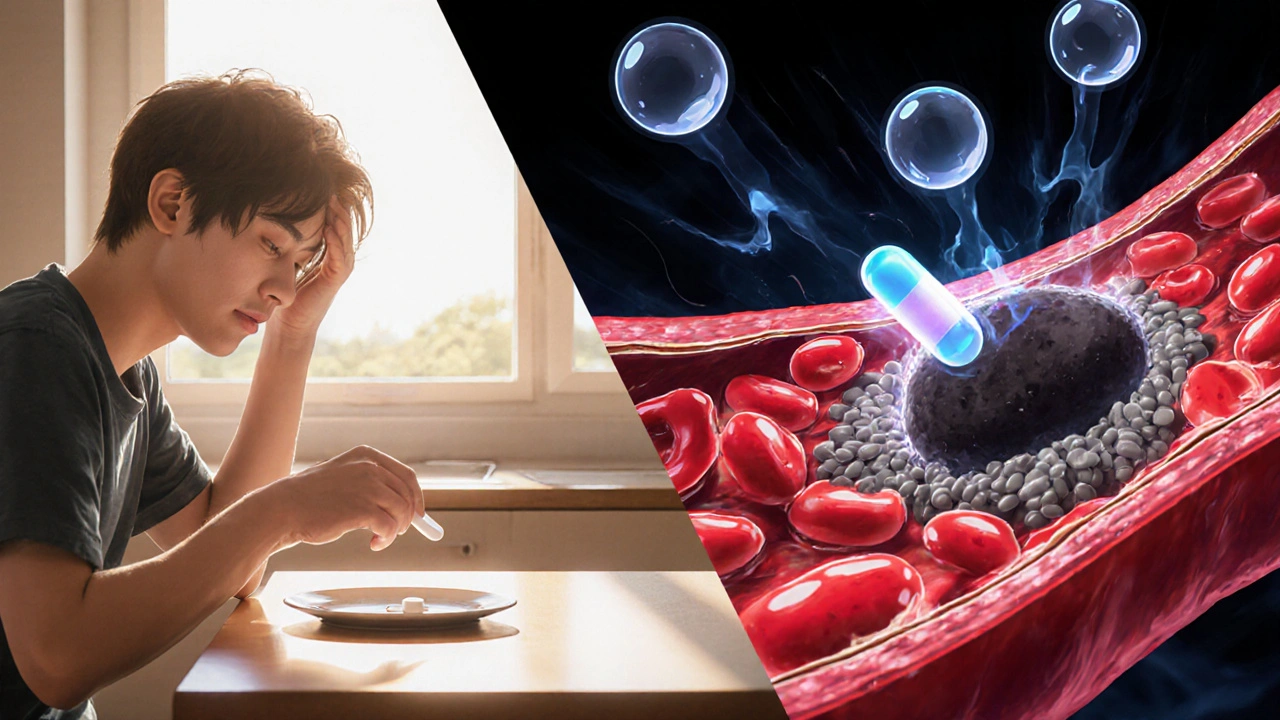
When working with embolism treatment, the set of medical approaches used to dissolve, remove, or prevent blood clots that block blood vessels. Also known as clot management, it plays a crucial role in conditions such as pulmonary embolism, a blockage in the lung arteries that can be life‑threatening and deep vein thrombosis, a clot forming in the deep veins of the legs. Effective care usually starts with anticoagulant therapy, medications like warfarin, rivaroxaban, or apixaban that stop the clot from growing. In many cases, doctors add thrombolytic therapy, drugs such as alteplase that actively break down the clot when rapid removal is needed. Those three entities—embolism treatment, anticoagulant therapy, and thrombolytic therapy—form a core triangle: embolism treatment encompasses anticoagulant therapy, requires timely diagnosis, and relies on thrombolytic therapy to improve outcomes. Beyond medication, some patients need surgical embolectomy or catheter‑based interventions, especially when the clot is large or located in a critical vessel. Lifestyle changes—like staying active, maintaining a healthy weight, and using compression stockings—support the medical plan and reduce the chance of recurrence.
Choosing the right approach begins with understanding the type of embolism. For embolism treatment of a pulmonary embolism, doctors often start with low‑molecular‑weight heparin followed by a direct oral anticoagulant, monitoring oxygen levels and heart function closely. In deep vein thrombosis, compression therapy and early mobilization complement anticoagulation, cutting down swelling and pain. When clot burden is high, interventional radiology can deliver catheter‑directed thrombolysis, delivering the drug straight to the blockage while minimizing systemic exposure. Surgical embolectomy remains an option for unstable patients who cannot receive clot‑busting drugs. Each method has distinct risks—bleeding with anticoagulants, allergic reactions with thrombolytics, or infection after surgery—so clinicians weigh benefits against individual health factors such as renal function, age, and bleeding history. Follow‑up imaging, usually a CT scan for pulmonary cases or an ultrasound for DVT, confirms that the clot has resolved or shrunk, guiding the duration of therapy, which can range from three months to indefinite use.
Understanding these options helps you ask the right questions during doctor visits: Will I need a blood thinner for life? How soon can I move around after treatment? What signs signal a complication? The articles below dive deeper into specific drugs, compare alternatives, and offer step‑by‑step guides on safe online purchases of common prescriptions. Browse the collection to find practical advice that matches your situation, whether you’re dealing with a fresh clot, managing long‑term therapy, or exploring preventive measures.