Aspirin Dosage Calculator
Determine Your Appropriate Aspirin Dosage
This tool helps you understand the recommended aspirin dosage based on your medical condition and risk factors. Always consult your healthcare provider before starting or changing medication.
Select options above to see your recommended dosage.
When you hear the word aspirin, you probably picture a cheap painkiller for headaches. Yet its role goes far beyond easing a sore temple. For decades doctors have leaned on aspirin to stop dangerous clots that can cause embolisms - sudden blockages that cut off blood flow to vital organs. This article unpacks exactly how aspirin helps prevent and treat embolism, what risks you should watch, and when other drugs might be a better fit.
What Aspirin Is and How It Works
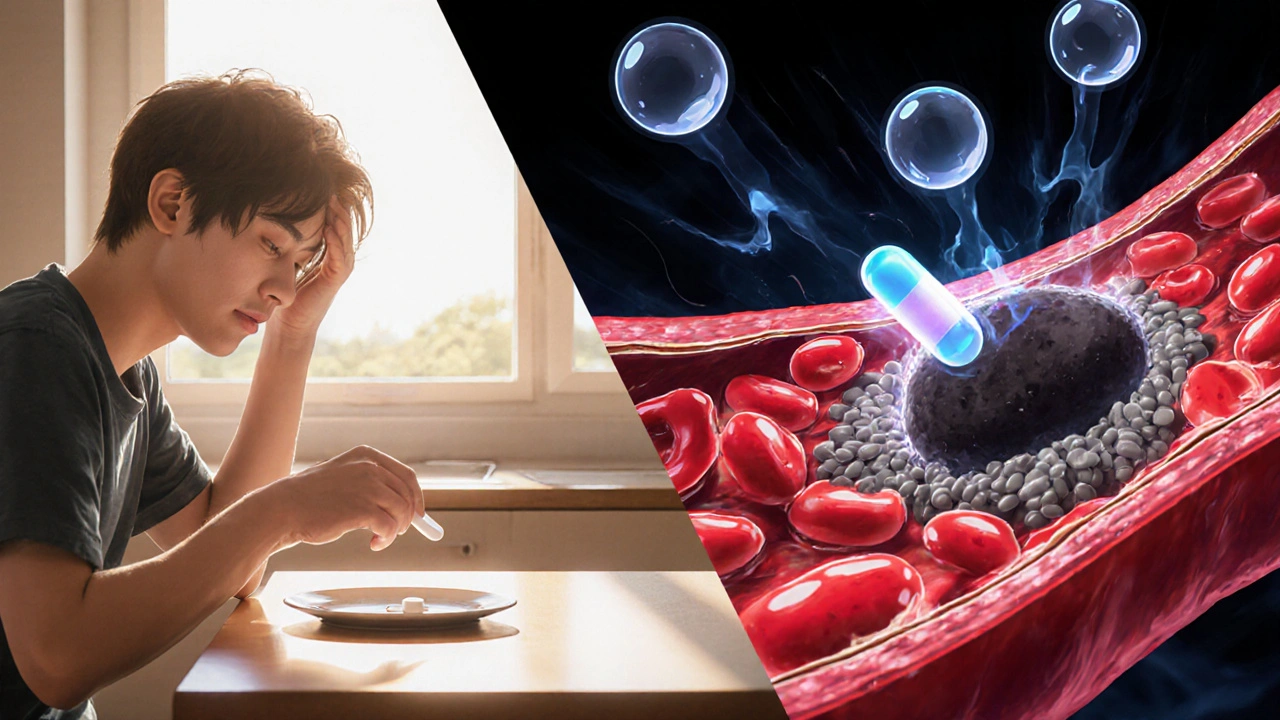
Aspirin is a salicylate drug that irreversibly inhibits the enzyme cyclooxygenase‑1 (COX‑1), reducing the production of thromboxane A2 - a molecule that tells platelets to stick together. By blocking thromboxane A2, aspirin dampens platelet aggregation, the first step in clot formation. The effect lasts for the lifespan of a platelet (about 7‑10 days), which means a single daily dose can keep the blood less “sticky” for a full week.
The anti‑inflammatory and antipyretic properties that make aspirin popular for colds are side effects of the same COX inhibition, but it’s the antiplatelet action that matters for embolism.
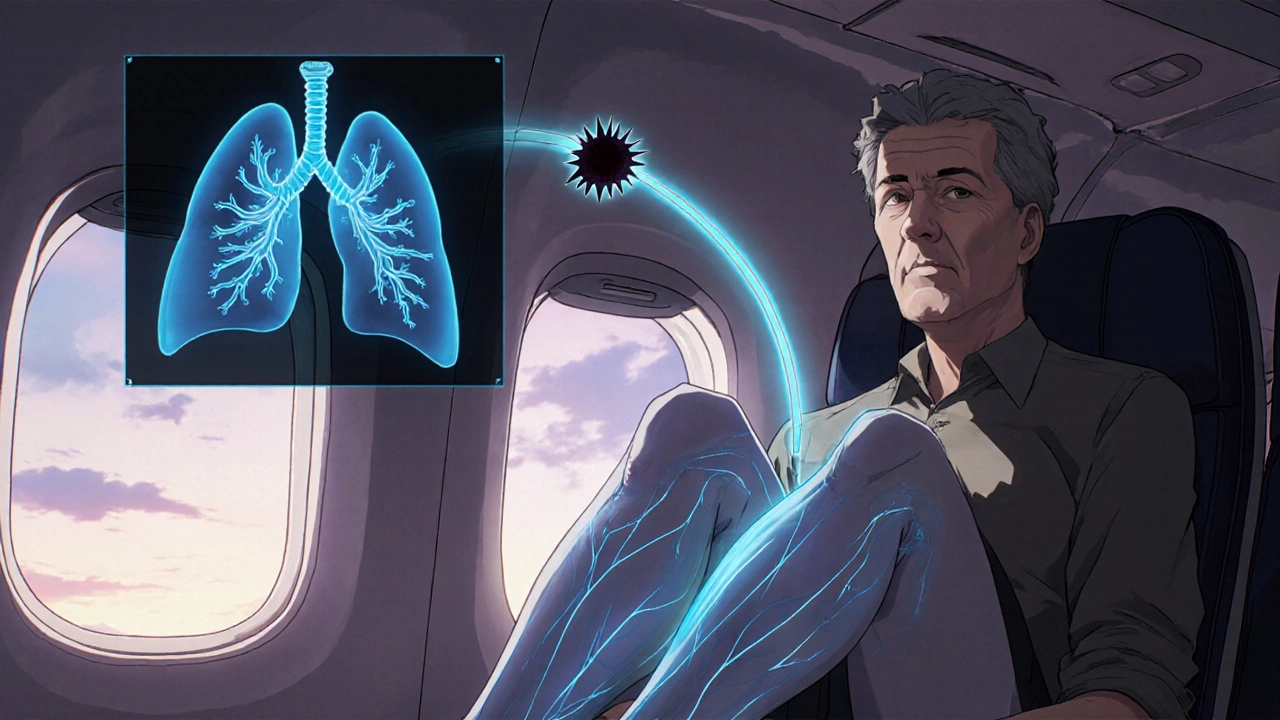
Understanding Embolism: Types and Risks
Embolism is a condition where a clot, air bubble, fat globule, or other material travels through the bloodstream and lodges in a vessel, abruptly blocking blood flow. The blockage can starve brain tissue (stroke), lung tissue (pulmonary embolism), or limbs (acute limb ischemia). Most emboli start as blood clots that form in the deep veins of the legs - a condition known as deep vein thrombosis (DVT) - before breaking free and traveling to the lungs.
Key risk factors include prolonged immobility (long flights, surgery), cancer, hormonal therapy, and inherited clotting disorders. Age, smoking, high cholesterol, and hypertension add to the danger, especially for cardiovascular disease.
Aspirin in Embolism Prevention
Because aspirin thins platelets, it’s most effective against clots that originate from platelet‑rich areas, like arteries. For venous clots (DVT and subsequent pulmonary embolism), the clot is fibrin‑rich and often needs anticoagulants such as warfarin or direct oral anticoagulants (DOACs). Still, low‑dose aspirin (75‑100 mg daily) can lower the risk of a first heart attack or ischemic stroke, which are common embolic events.
- Primary prevention of ischemic stroke: Large meta‑analyses (e.g., Antithrombotic Trialists’ Collaboration, 2022) show a 9 % relative risk reduction in first‑time ischemic stroke for patients aged 50‑70 with at least one cardiovascular risk factor.
- Secondary prevention after a heart attack: Guidelines from the American College of Cardiology (ACC) recommend 81 mg aspirin indefinitely unless contraindicated.
- Post‑surgical prophylaxis: For patients undergoing orthopedic knee or hip replacement, aspirin (325 mg BID for 5‑7 days) is an accepted alternative to stronger anticoagulants when bleeding risk is high.
It’s crucial to match aspirin’s strengths with the right embolic threat. For pure venous thromboembolism (VTE) prevention, studies like the WARFASA trial (2021) found aspirin less effective than DOACs, but still better than placebo.
Aspirin in Embolism Treatment
When an embolism has already occurred, aspirin’s role shifts to preventing new clots rather than dissolving the existing blockage. Acute treatment of a stroke caused by a clot (ischemic stroke) usually involves thrombolytics (tPA) or mechanical thrombectomy. After the acute phase, aspirin (usually 325 mg once daily) is started within 24‑48 hours to curb recurrent events.
For myocardial infarction (heart attack), aspirin is given immediately - often a chewable 162‑300 mg dose - to stop platelet growth at the culprit artery. Follow‑up therapy combines aspirin with a second antiplatelet (dual antiplatelet therapy, DAPT) for 6‑12 months, especially after stent placement.
In pulmonary embolism, anticoagulants remain the cornerstone. However, once a patient transitions to long‑term oral anticoagulation, many clinicians add low‑dose aspirin if the patient also has coronary artery disease, balancing clot prevention against bleeding risk.
Dosage, Safety, and Who Should Avoid Aspirin
Typical dosing for embolism‑related use:
- Primary prevention: 75‑100 mg daily (often called “baby aspirin”).
- Secondary prevention (post‑MI or stroke): 81‑325 mg daily, depending on physician judgment.
- Acute coronary syndrome: 162‑300 mg chewable loading dose, then 81‑325 mg daily.
Safety considerations are vital. Aspirin can irritate the stomach lining, leading to gastritis or bleeding. People with a history of peptic ulcer disease, uncontrolled hypertension, or active bleeding should discuss alternatives. Children and teenagers with viral infections should avoid aspirin due to the risk of Reye’s syndrome.
Renal impairment, liver disease, and severe asthma (aspirin‑exacerbated respiratory disease) are additional red flags. In these cases, doctors may prescribe clopidogrel or a DOAC instead.
How Aspirin Stacks Up Against Other Blood‑Thinning Options
| Drug | Mechanism | Typical Dose for Embolism Prevention | Key Advantages | Main Risks |
|---|---|---|---|---|
| Aspirin | Irreversible COX‑1 inhibition → ↓ platelet aggregation | 75‑100 mg daily (primary); 81‑325 mg daily (secondary) | Cheap, widely available, long track record | GI bleeding, ulcer, Reye’s syndrome in kids |
| Clopidogrel | P2Y12 ADP‑receptor blocker → ↓ platelet activation | 75 mg daily | Less GI irritation, useful when aspirin intolerant | Bleeding, rare thrombotic thrombocytopenic purpura |
| Warfarin | Vitamin K antagonist → ↓ clotting factor synthesis | Target INR 2‑3 (dose varies) | Effective for VTE, can be reversed with vitamin K | Frequent monitoring, diet interactions, bleeding |
| Apixaban (DOAC) | Factor Xa inhibitor → ↓ thrombin generation | 5 mg BID (adjusted for renal function) | No routine labs, quick onset, lower intracranial bleed risk | Cost, contraindicated in severe renal impairment |
| Heparin (IV/SC) | Activates antithrombin III → ↓ clotting factors II, IX, X | Weight‑based dosing (e.g., 5,000 U SC BID) | Rapid anticoagulation, easy bridge to oral agents | Heparin‑induced thrombocytopenia, monitoring needed |
The table shows that aspirin shines when cost, ease of use, and long‑term safety matter. When a patient needs strong anticoagulation - such as after a confirmed DVT/PE - a DOAC or warfarin is usually the better choice.
Practical Checklist for Using Aspirin Safely
- Confirm the indication: primary prevention (low‑dose) vs. secondary prevention (higher dose).
- Screen for GI risk factors - past ulcers, NSAID use, chronic steroids.
- Check for bleeding disorders or current anticoagulant therapy.
- Ask about asthma or nasal polyps (possible aspirin‑exacerbated respiratory disease).
- Determine renal and hepatic function if considering higher doses.
- Set a reminder to take aspirin at the same time each day to maintain steady platelet inhibition.
- Schedule regular follow‑up labs if you’re on dual therapy (e.g., aspirin + clopidogrel) to watch hemoglobin and platelet counts.
Following the checklist helps you reap aspirin’s clot‑preventing benefits while sidestepping the most common side effects.
Frequently Asked Questions
Can aspirin replace blood thinners after a pulmonary embolism?
No. Aspirin mainly inhibits platelets, while pulmonary embolism is usually a fibrin‑rich clot that needs anticoagulation (warfarin, DOACs, or heparin). Aspirin may be added later if the patient also has coronary artery disease, but it’s not a substitute for primary PE treatment.
Is low‑dose aspirin safe for people over 80?
Evidence is mixed. The ASPREE trial (2021) showed that healthy adults ≥ 70 years who took 100 mg daily had higher overall mortality due to bleeding. For those with established cardiovascular disease, the benefit may still outweigh risk, but clinicians usually individualize the decision.
How long does aspirin’s antiplatelet effect last after stopping?
Because aspirin irreversibly disables COX‑1 in each platelet, the effect lasts until the body produces new platelets - roughly 7‑10 days. Doctors often advise a 10‑day washout before surgery.
Should I take aspirin with food?
Yes. Taking it with a meal or a full glass of water reduces stomach irritation. Some patients also use a proton‑pump inhibitor (e.g., omeprazole) if they have a history of ulcers.
Can aspirin cause a stroke?
Rarely. In people with hemorrhagic stroke risk (e.g., uncontrolled hypertension), aspirin’s bleed‑promoting effect can worsen bleeding. That’s why blood‑pressure control is essential before starting therapy.


8 Comments
alex montana October 18, 2025 AT 19:54
Aspirin is not just a cheap headache fix, it’s a double‑edged sword that can swing either way! It irreversibly blocks COX‑1, halting thromboxane production, which means platelets can’t clump together?? Because platelets live for about a week, a single daily tablet keeps the blood less sticky for days... But the same mechanism that prevents clots also gnaws at the stomach lining, inviting ulcers!!! Patients with a history of GI bleeding must weigh the risk versus the benefit, and often they don’t!!! In primary prevention for folks over 50, the modest 9 % risk reduction can be dwarfed by bleeding incidents... When you combine aspirin with a proton‑pump inhibitor, you mute the gastric assault, yet you add another drug to the mix?? Doctors sometimes prescribe low‑dose “baby aspirin” for arterial protection, yet they hesitate for venous clot scenarios because fibrin‑rich clots need anticoagulants!!! The literature shows that for deep‑vein thrombosis prevention, aspirin lags behind DOACs, but it still beats placebo... If you’re post‑orthopedic surgery and bleeding risk is high, aspirin becomes an attractive alternative to warfarin!!! Remember, the antiplatelet effect lasts for the lifespan of each platelet-about 7‑10 days-so stopping aspirin doesn’t erase its influence instantly... Guidelines advise a 10‑day washout before major surgery to avoid intra‑operative bleeding... Some patients report mild dyspepsia, while others experience severe hemorrhage, a stark reminder of the fine line we walk... Aspirin’s price and accessibility make it appealing, yet the hidden costs of GI complications can burden the healthcare system!!! Bottom line: aspirin can be a lifesaver when used correctly, but misuse can turn it into a silent killer...
Wyatt Schwindt October 19, 2025 AT 00:04
The article explains the mechanisms clearly
Fabian Märkl October 19, 2025 AT 04:14
I love how the piece breaks down the science without drowning you in jargon 😊
Knowing that low‑dose aspirin can shave off a few percent of stroke risk makes the decision feel more concrete 🚀
At the same time, the reminder about GI risks keeps us honest about the trade‑offs 🙏
If you’re on other blood thinners, the article’s note on adding aspirin only when there’s coronary disease is spot on!
Overall, it’s a balanced guide that empowers patients to talk to their doctors with confidence.
Natala Storczyk October 19, 2025 AT 08:24
This so‑called “cheap painkiller” is being weaponized by big pharma!!!
They hide the bleeding dangers while pushing pills like candy!!!
Don’t be fooled by glossy guidelines that praise aspirin for “prevention”!!!
The hidden agenda is clear: sell you a pill, reap the profits, then fix the fallout with more drugs!!!
Wake up and read the fine print, or you’ll end up bleeding on the battlefield of health!!!
Karla Johnson October 19, 2025 AT 12:34
Aspirin’s role in embolism management is a nuanced subject that intertwines pharmacodynamics, epidemiology, and individualized patient risk assessment, and it deserves a thorough exploration. The irreversible inhibition of cyclooxygenase‑1 means that each platelet exposed to the drug remains silenced for its entire lifespan, which can be as long as ten days, thereby providing a sustained antiplatelet effect. This mechanism is particularly effective in arterial territories where platelet‑rich thrombi precipitate events like myocardial infarction and ischemic stroke, conditions that dominate the morbidity statistics in older populations. Conversely, venous thromboembolism typically arises from fibrin‑rich clots, where platelets play a secondary role, making direct anticoagulants such as warfarin, apixaban, or rivaroxaban more appropriate therapeutic agents. Clinical trials, including the WARFASA and ASCEND studies, have consistently shown that low‑dose aspirin reduces the incidence of first‑time vascular events, yet the absolute benefit often pales in comparison to the increased risk of gastrointestinal bleeding. When prescribing aspirin for primary prevention, physicians must employ a calibrated risk‑benefit algorithm, incorporating factors like age, hypertension, diabetes, smoking status, and prior ulcer disease. For patients with established coronary artery disease, the evidence is more unequivocal; lifelong low‑dose aspirin, often paired with a second antiplatelet such as clopidogrel in a dual antiplatelet regimen, markedly lowers the recurrence of ischemic events. The timing of aspirin initiation after an acute coronary syndrome is also critical; a chewable loading dose of 162‑300 mg administered promptly can halt platelet aggregation at the culprit lesion, while subsequent maintenance doses maintain the therapeutic window. In the postoperative setting, especially after orthopedic joint replacement, the balance shifts again; while aspirin offers a convenient oral prophylaxis with a lower bleeding profile than potent anticoagulants, many surgeons still favor DOACs for high‑risk patients. The gastrointestinal safety profile of aspirin can be mitigated by co‑prescribing proton‑pump inhibitors, which shield the mucosa from acid‑mediated injury, but this adds complexity and cost to the regimen. Patient education remains a cornerstone; individuals should be advised to take aspirin with food, avoid alcohol excess, and report any signs of melena or unexplained bruising promptly. Renal and hepatic function tests should be monitored when higher doses are employed, particularly in patients with comorbidities that predispose them to drug accumulation. In practice, the decision to employ aspirin must be revisited periodically, as evolving comorbid conditions, changes in concomitant medications, and emerging evidence can tip the scales toward either continuation or cessation. Overall, aspirin shines as an accessible, cost‑effective tool for arterial thrombosis prevention, but its utility in venous clot prophylaxis is limited and should be complemented-or replaced-by agents that target the coagulation cascade directly. Thus, the clinician’s role is not merely to prescribe a pill but to integrate a comprehensive risk assessment, patient preferences, and the latest guideline updates to craft a personalized therapeutic plan.
Ayla Stewart October 19, 2025 AT 16:44
Aspirin can be useful for heart health if taken at a low dose, but you should check for stomach problems first. It’s also important to talk with a doctor before mixing it with other blood thinners.
Liberty Moneybomb October 19, 2025 AT 20:54
The mainstream narrative about aspirin being a harmless over‑the‑counter drug is a smokescreen crafted by the pharmaceutical elite. They want you to think a cheap tablet will protect you while they profit from treating the complications they create. Keep an eye on the hidden clauses in the guidelines – they often favor big‑drug interests over true patient safety. Remember, questioning the official recommendations is the first step toward real health autonomy.
Alex Lineses October 20, 2025 AT 01:04
From a pharmacologic standpoint, aspirin’s irreversible COX‑1 inhibition reduces thromboxane A₂ synthesis, thereby attenuating platelet aggregation. In patients with established atherothrombotic disease, integrating aspirin into a dual antiplatelet regimen-typically with a P2Y₁₂ inhibitor-optimizes secondary prevention outcomes. When co‑prescribed with anticoagulants, clinicians must monitor for synergistic bleeding risk, adjusting the therapeutic index accordingly. Utilizing risk stratification tools such as HAS-BLED can guide the decision-making process and ensure evidence‑based management.