When talking about embolism prevention, the set of actions and treatments that lower the chance of a blood clot traveling to vital organs. Also known as clot prevention, it combines medical, dietary and activity‑based steps. Embolism prevention is not a one‑size‑fits‑all plan; it adapts to each person’s health profile.
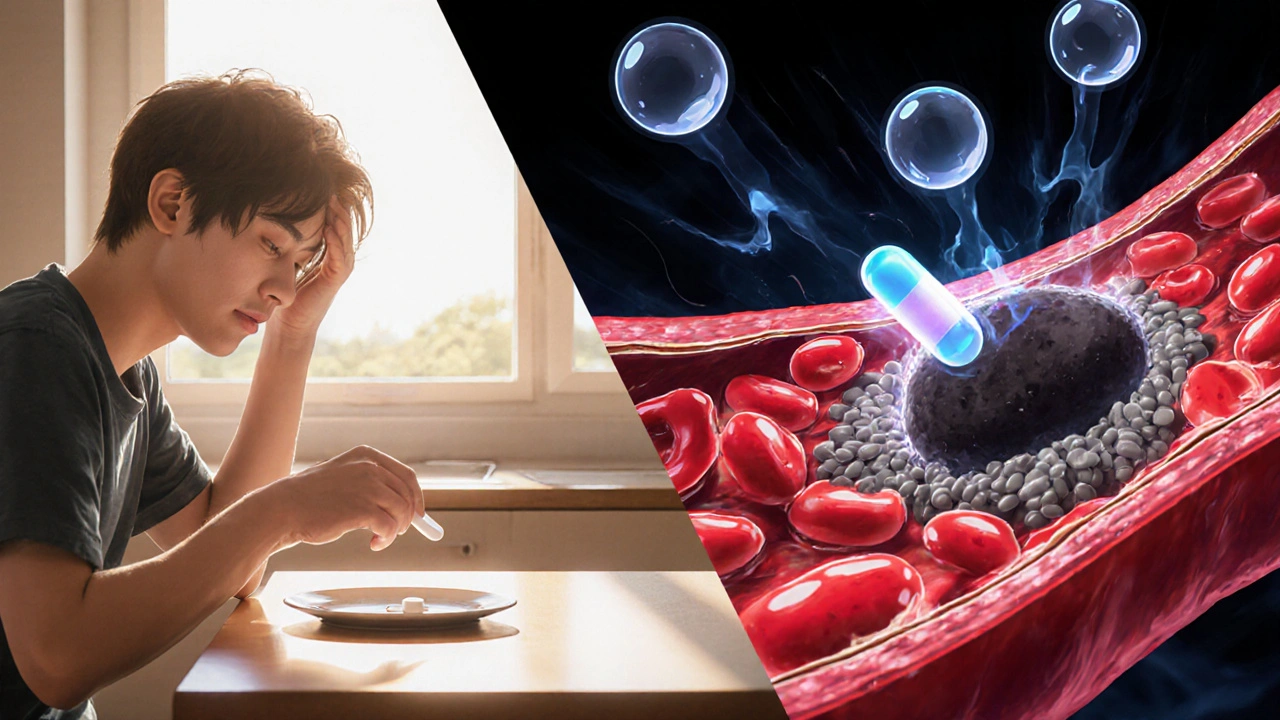
One of the pillars is anticoagulant therapy, medications that thin the blood and stop clots from forming or growing. Doctors often prescribe these after surgery, during a heart condition, or when a patient shows early signs of clotting. Another key piece is understanding deep vein thrombosis, a clot that builds up in the deep veins of the legs. DVT is a major trigger for pulmonary embolism, when a clot breaks free and blocks an artery in the lungs, a life‑threatening event. Recognizing that deep vein thrombosis increases pulmonary embolism risk helps you target prevention where it matters most.
Beyond meds, lifestyle choices shape the risk landscape. Keeping a healthy weight, staying active, and avoiding prolonged immobility (like long flights) cut down the chance of a clot forming. Hydration and leg‑raising exercises are simple habits that many people overlook but prove effective. Likewise, identifying blood clot risk factors, such as smoking, genetic clotting disorders, or certain cancers lets you and your doctor craft a personalized plan. Effective embolism prevention requires anticoagulant therapy, lifestyle adjustments, and risk‑factor monitoring—a three‑way approach that covers the most common pathways to clot formation.
In the collection below you’ll find guides on specific drugs, how to manage side effects, and practical tips for everyday habits that lower clot risk. Whether you’re looking for medication comparisons or simple lifestyle tweaks, the articles ahead give you actionable insight to keep embolisms at bay.