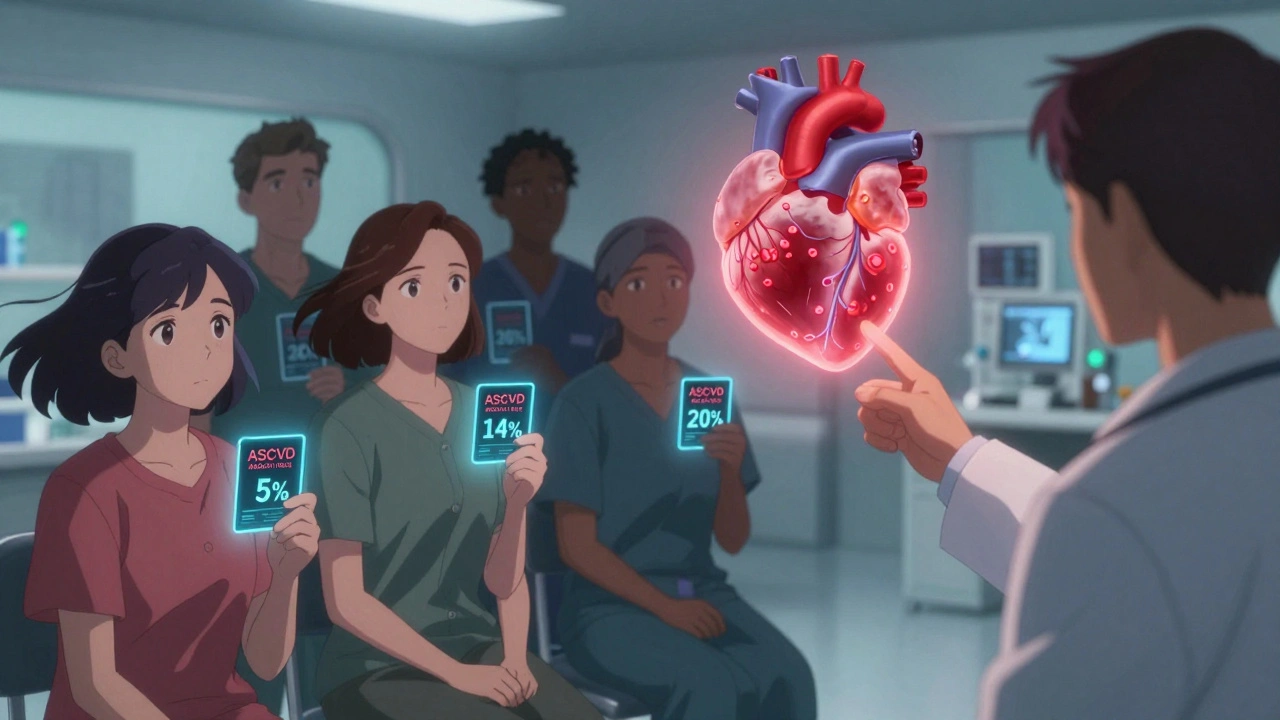
When you hear cardiac risk calculator, a tool that estimates your chance of having a heart attack or stroke over the next 10 years based on health data. It’s not magic—it’s math built from decades of clinical studies, like the ASCVD risk estimator used by the American Heart Association. This calculator takes your age, sex, race, blood pressure, cholesterol levels, diabetes status, and smoking habits, then spits out a percentage. That number? It tells you whether you’re at low, intermediate, or high risk for cardiovascular disease, the leading cause of death in the U.S.
Why does this matter? Because most people don’t know their real risk until they have a heart attack. A 55-year-old man with high LDL and borderline blood pressure might think he’s fine because he’s not overweight. But the calculator shows his 10-year risk is 18%. That’s not "maybe"—that’s a warning sign. Doctors use this tool to decide if you need statins, blood pressure meds, or just lifestyle changes. And it’s not just for older adults. People in their 30s and 40s with family history or prediabetes are seeing numbers that surprise them. The cholesterol levels you get from a simple blood test? They’re half the story. Your systolic pressure, whether you smoke, and if you have diabetes are just as important. These aren’t abstract numbers—they’re triggers for action.
You’ll find posts here that explain how ECG and stress tests fit into the bigger picture of heart health, what black box warnings mean for heart meds, and how HIV drugs can mess with your cholesterol. There’s advice on statins that are safe with HIV treatment, how hypertension meds interact with OTC painkillers, and why dual antiplatelet therapy after a stent requires careful balancing. All of it connects back to one thing: knowing your risk isn’t enough—you need to act on it. The cardiac risk calculator is your starting line. The posts below show you what to do next.