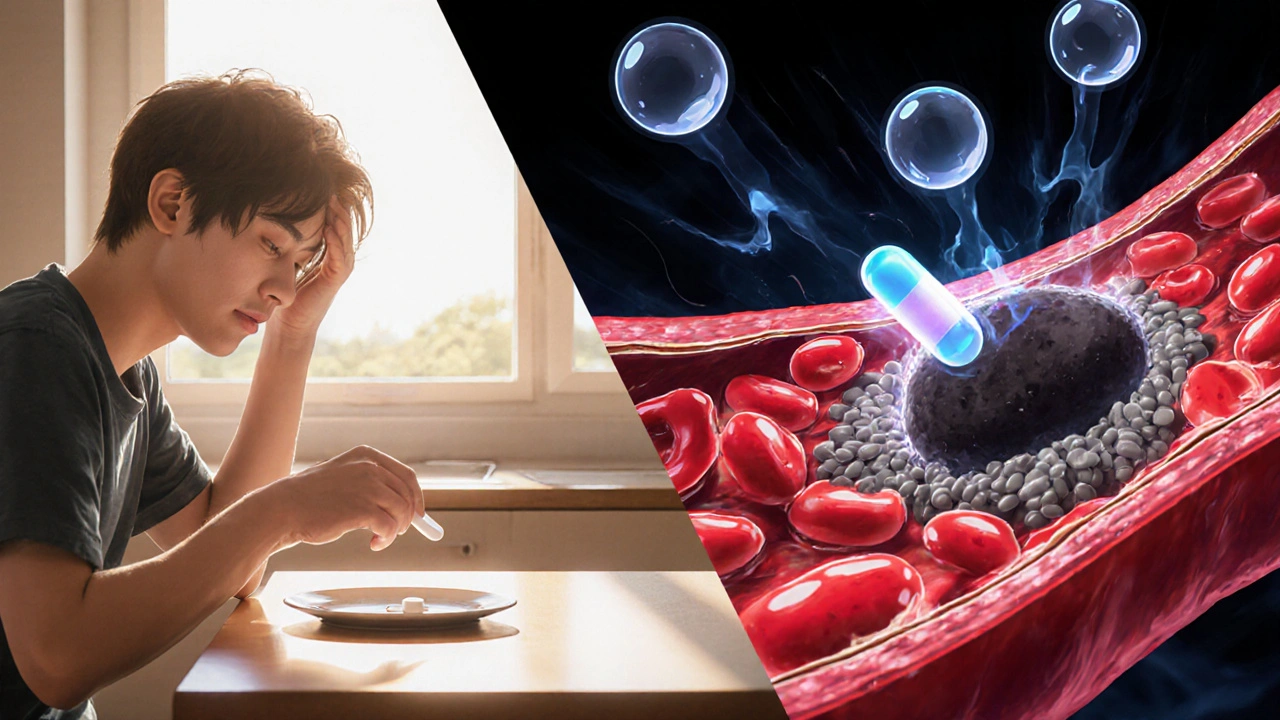
When talking about antiplatelet therapy, a treatment strategy that blocks platelets from forming clots in the bloodstream. Also known as platelet inhibition, it is a cornerstone of modern cardiovascular care and is prescribed to patients at risk of heart attack, stroke, or peripheral artery disease.
Platelets are tiny blood cells that rush to seal any break in a vessel wall. When they stick together too readily, they form a blockage called a thrombus. This process, called platelet aggregation, is the engine behind most acute coronary events. By interfering with the chemicals that tell platelets to clump, antiplatelet drugs lower the chance that a clot will block a coronary artery or a cerebral vessel.
Two common pathways are targeted: the cyclooxygenase‑1 (COX‑1) pathway, which aspirin blocks, and the P2Y12 receptor, which clopidogrel and newer agents inhibit. Understanding which pathway dominates in a given patient helps doctors pick the right medication and dose.
Beyond the basic drugs, the concept of dual antiplatelet therapy (DAPT) has reshaped heart‑procedure care. DAPT pairs aspirin with a P2Y12 inhibitor to give a stronger, yet still safe, clot‑prevention effect. The combination is especially useful after stent placement, where the metal scaffold can trigger platelet activation.
Stents are tiny tubes that keep narrowed arteries open after angioplasty. The metal surface can be a focus for platelet attachment, so doctors usually prescribe DAPT for at least one month after a drug‑eluting stent and up to a year after a bare‑metal stent. Research shows that patients who stop DAPT too early face a higher risk of stent thrombosis, a serious event that can cause heart attack.
Antiplatelet therapy does more than protect stents. It is also a mainstay in managing cardiovascular disease broadly. People with stable angina, recent myocardial infarction, or ischemic stroke often receive long‑term aspirin or a P2Y12 inhibitor. The therapy reduces the odds of a second event by roughly 20‑25% in large trials.
Choosing the right regimen involves weighing benefits against bleeding risk. Older adults, patients with a history of gastrointestinal ulcers, or those on anticoagulants need special attention. Many clinicians add a proton‑pump inhibitor to protect the stomach when prescribing aspirin, and they may monitor platelet function in high‑risk cases.
In the collection below, you’ll find practical guides that break down each drug, compare aspirin with newer agents, explain how DAPT works after stent procedures, and share tips for balancing clot prevention with bleeding concerns. Whether you’re a patient looking to understand your prescription or a caregiver seeking clear answers, this roundup gives you the facts you need to make informed decisions about antiplatelet therapy and keep your heart running smoothly.