When you have an autoimmune disease, a condition where the immune system mistakenly attacks the body’s own tissues. Also known as autoimmune disorder, it can include lupus, rheumatoid arthritis, Hashimoto’s thyroiditis, and multiple sclerosis. Pregnancy doesn’t cure it—but it can change how it acts. Some women feel better during pregnancy, especially with rheumatoid arthritis or multiple sclerosis. Others, like those with lupus, face higher risks of flare-ups, preterm birth, or preeclampsia. The key? Planning ahead and knowing what’s safe.
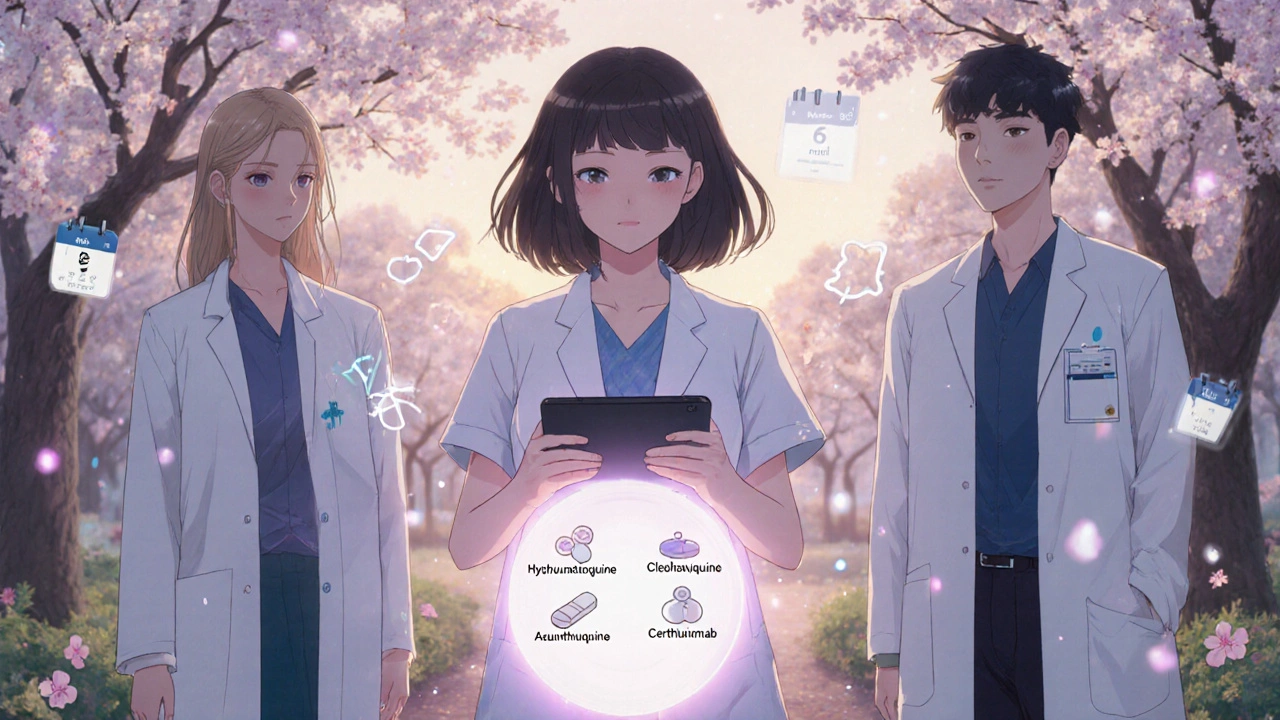
It’s not just about the disease itself. The medications, drugs used to control autoimmune symptoms. Also known as immunosuppressants, it includes drugs like prednisone, hydroxychloroquine, and azathioprine. you take matter just as much. Some are safe during pregnancy—like hydroxychloroquine for lupus. Others, like methotrexate or mycophenolate, can cause serious birth defects and must be stopped months before trying to conceive. Your doctor won’t just look at your disease—they’ll look at every pill in your cabinet. And it’s not just prescriptions. Supplements like high-dose fish oil or turmeric might help reduce inflammation, but they can also interact with your meds or affect bleeding risk during delivery.
Then there’s the immune system, the body’s defense network that normally protects against infection. Also known as immune response, it shifts dramatically during pregnancy to protect the fetus.. It doesn’t shut down—it recalibrates. That’s why some autoimmune symptoms improve: the body is less aggressive toward foreign tissue, including the baby. But that same shift can make you more vulnerable to infections like the flu or UTIs, which can trigger flares. Monitoring isn’t optional. Regular blood tests, urine checks, and ultrasounds aren’t just routine—they’re lifesavers.
Many women with autoimmune conditions have healthy pregnancies. But it takes teamwork: your OB-GYN, rheumatologist, and pharmacist all need to be on the same page. You can’t just Google "safe meds during pregnancy"—the answers change based on your specific disease, how active it is, and what stage you’re in. That’s why the posts below cover real cases: how lupus patients managed flares in the third trimester, why some women had to switch from biologics before conceiving, how thyroid levels must be tracked monthly, and what to do if you get sick while on immunosuppressants. You’ll find practical advice on diet, stress, and monitoring—not theory. Just what works, when it matters most.