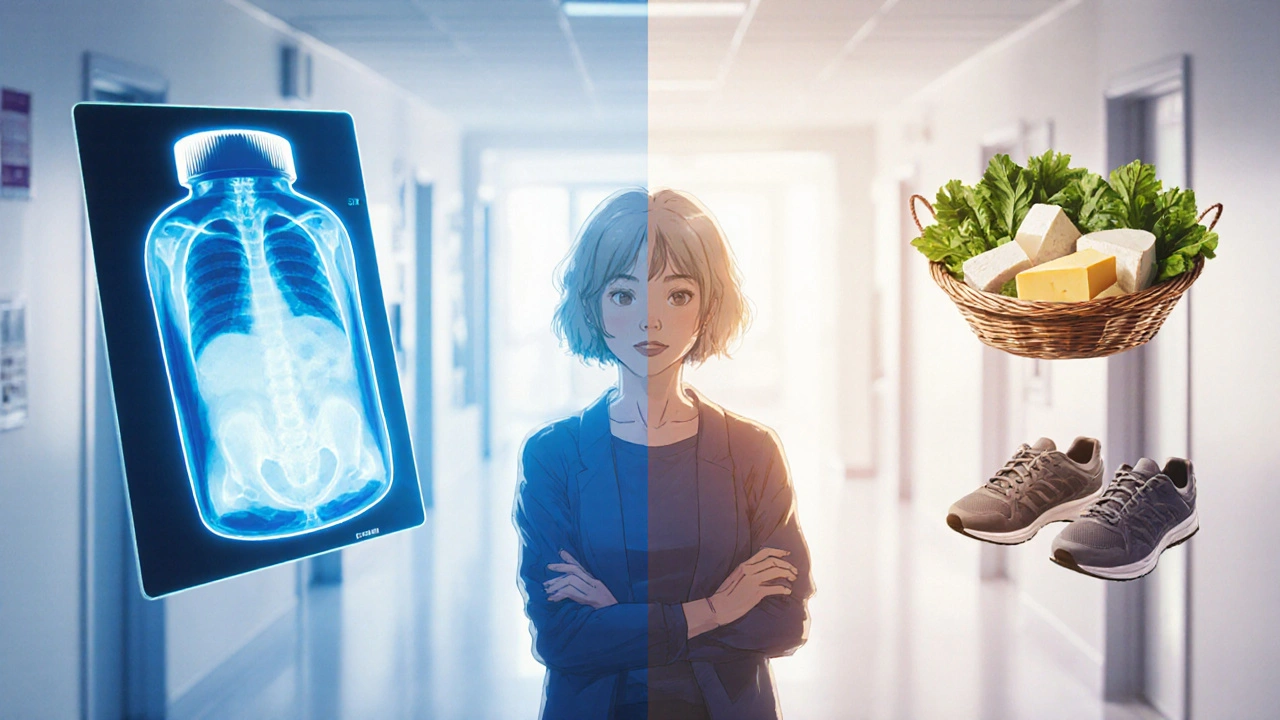
When dealing with osteoporosis treatment, a set of medical and lifestyle strategies aimed at strengthening weak bones and lowering fracture risk. Also known as bone loss therapy, it requires a clear picture of what works best for each person. Understanding the big picture lets you choose the right mix of meds, nutrients, and activity. That's why a solid osteoporosis treatment plan feels like putting together a puzzle where every piece matters.
Prescription drugs are often the backbone of any osteoporosis plan. bisphosphonates, drugs that slow bone breakdown and can even help build new bone over time are the most common first‑line option. They work by attaching to bone surfaces and inhibiting the cells that chew away bone tissue. Another powerful class is hormone‑based therapy; hormone therapy, estrogen or selective estrogen‑receptor modulators that help maintain bone density in post‑menopausal women can be a good fit when bisphosphonates aren’t tolerated. Newer monoclonal antibodies, such as denosumab, add another tool for people who need a different mechanism. The key semantic link here is that effective medication requires a match between the drug’s action and the patient’s specific bone‑loss pattern.
But drugs alone aren’t enough. Your body needs the right building blocks to respond to treatment, and that’s where nutrition steps in.
Calcium is the primary mineral in bone, so a calcium supplement, often calcium carbonate or citrate taken to meet daily intake goals helps fill any dietary gaps. Most guidelines suggest 1,000–1,200 mg per day for adults at risk. Pair that with vitamin D, the vitamin that boosts calcium absorption in the gut, typically 800–1,000 IU daily, and you give your skeleton the raw material it needs to rebuild. The semantic triple: adequate calcium intake enables vitamin D to enhance bone mineralization, which in turn supports medication effectiveness.
Beyond pills, everyday food choices matter. Dairy, leafy greens, fortified plant milks, and fatty fish all pack calcium and vitamin D. Watching sodium and caffeine is wise, as they can increase calcium loss.
Now, let’s talk about the physical side of strengthening bones.
Weight‑bearing exercise is a cornerstone of any osteoporosis regimen. weight‑bearing exercise, activities like walking, dancing, or light jogging that force the skeleton to support the body’s weight sends mechanical signals that stimulate bone‑forming cells. When you add resistance training—think dumbbell curls, leg presses, or resistance bands—you boost muscle strength, which further protects bones from falls. The semantic relationship: regular weight‑bearing activity influences bone density, and stronger muscles reduce fracture risk.
Balance and flexibility drills, such as tai chi or yoga, complement the load‑bearing work. They improve coordination, making falls less likely—a crucial piece of the safety puzzle for anyone with fragile bones.
Monitoring progress lets you fine‑tune the plan. Bone mineral density (BMD) testing, usually via DXA scan, quantifies how much bone you have and tracks changes over time. Tools like the FRAX score estimate your 10‑year fracture risk based on age, gender, BMD, and other health factors. Regular labs—checking calcium, vitamin D, and kidney function—ensure that medications and supplements stay within safe limits.
Putting it all together, a personalized osteoporosis treatment strategy blends the right prescription, adequate calcium and vitamin D, targeted exercise, and ongoing monitoring. This integrated approach creates a feedback loop: meds improve bone structure, nutrients give the raw material, exercise reinforces strength, and tests tell you what to adjust.
Below you’ll find a curated collection of articles that dive deeper into each of these areas—drug comparisons, supplement guides, workout tips, and monitoring basics. Explore the posts to build a plan that fits your lifestyle, health profile, and goals, and turn the science of bone health into everyday action.