When working with NSAID alternatives, drugs or methods used instead of traditional non‑steroidal anti‑inflammatory medicines to relieve pain and reduce swelling. Also known as non‑NSAID pain relievers, it offers a route that sidesteps many of the stomach and cardiovascular risks linked to classic NSAIDs.
One of the most common substitutes is acetaminophen, an analgesic that works mainly in the brain to lower pain signals without directly blocking inflammation pathways. Because it doesn’t inhibit cyclo‑oxygenase enzymes, acetaminophen avoids the gastric irritation typical of ibuprofen or naproxen. However, high doses can stress the liver, so dosing limits are crucial. NSAID alternatives often start with acetaminophen when the primary goal is pain relief rather than strong anti‑inflammatory action.
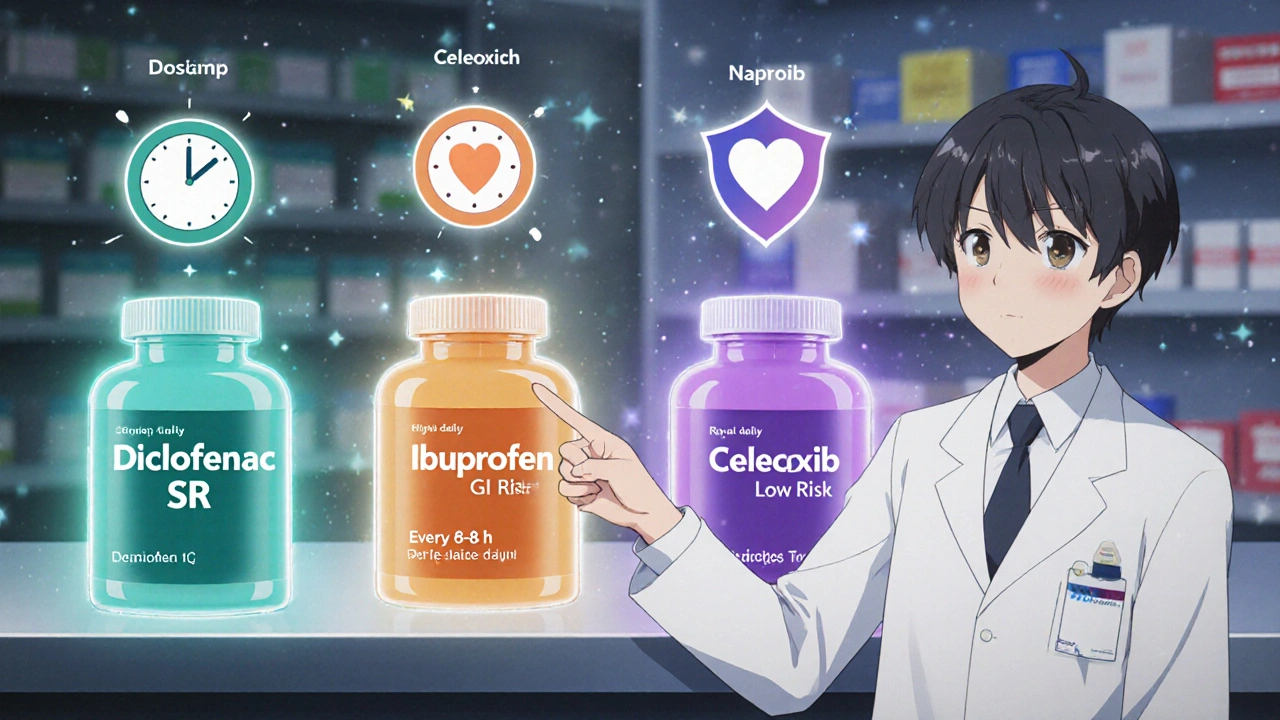
For patients who need anti‑inflammatory power but can’t tolerate traditional NSAIDs, COX‑2 inhibitors, selective drugs that block the cyclo‑oxygenase‑2 enzyme responsible for inflammation while sparing COX‑1, which protects the stomach lining become a viable option. Celecoxib is the most well‑known example; it provides joint pain relief with a lower risk of ulceration. Still, COX‑2 inhibitors carry their own cardiovascular warnings, so doctors weigh heart health against joint benefits. This choice illustrates the semantic triple: NSAID alternatives encompass COX‑2 inhibitors, which require careful cardiovascular assessment.
Beyond pills, many topical pain relievers, creams, gels or patches applied directly to the skin that deliver anti‑inflammatory agents locally serve as NSAID alternatives. Ingredients like diclofenac gel, menthol, or capsaicin can reduce knee or elbow pain without systemic exposure. Because the drug stays near the site of injury, systemic side effects stay minimal. Selecting a topical option often hinges on the pain’s location and the skin’s tolerance—if a patient experiences dermatitis from creams, an oral or natural route may be better.
Natural supplements also enter the conversation. omega‑3 fatty acids, polyunsaturated fats that modulate inflammatory pathways and can lower joint swelling and turmeric’s curcumin have modest anti‑inflammatory effects. These agents influence inflammation and can serve as NSAID alternatives for people seeking a non‑pharmaceutical route. The triple here is clear: supplements influence inflammation and can act as NSAID alternatives, offering a gentler but slower-acting approach.
Non‑drug strategies round out the toolbox. Physical therapy, weight management, and ergonomic adjustments reduce mechanical stress on joints, which in turn lowers the need for any medication. A balanced diet rich in antioxidants supports the body’s natural healing processes. When pain stems from overuse or poor posture, these lifestyle tweaks often replace the need for medication altogether. This demonstrates that NSAID alternatives aren’t limited to pills—they include any method that helps manage pain and inflammation.
Safety remains the top priority. Every alternative comes with its own risk profile: acetaminophen’s liver toxicity, COX‑2 inhibitors’ heart concerns, topicals’ skin reactions, and supplements’ variable purity. Before swapping a prescribed NSAID, patients should discuss their medical history, current meds, and kidney or liver function with a healthcare provider. Understanding the trade‑offs lets you choose an alternative that aligns with your health goals. Choosing an NSAID alternative requires knowing the drug’s mechanism, the condition being treated, and personal risk factors.
Below you’ll find a curated selection of articles that dive deeper into these options. From detailed comparisons of aspirin and other blood thinners to guides on buying cheap generic pain relievers online, the posts cover everything you need to make an informed decision about pain management without traditional NSAIDs. Explore the full range of alternatives and pick the one that fits your situation best.