When comparing naproxen vs diclofenac, two widely used non‑steroidal anti‑inflammatory drugs (NSAIDs) that treat pain, inflammation, and arthritis, also known as NSAID comparison, you’re really looking at how each drug balances effectiveness, safety, and cost. Both belong to the broader class of NSAIDs, medications that reduce inflammation by inhibiting cyclooxygenase (COX) enzymes. Key concerns include gastrointestinal side effects, ulcers, bleeding, or stomach upset that can arise from long‑term NSAID use and cardiovascular risk, increased chances of heart attack or stroke linked to some NSAIDs. Understanding these three entities—naproxen vs diclofenac, NSAIDs, and the safety profile—helps you decide which option fits your health goals.
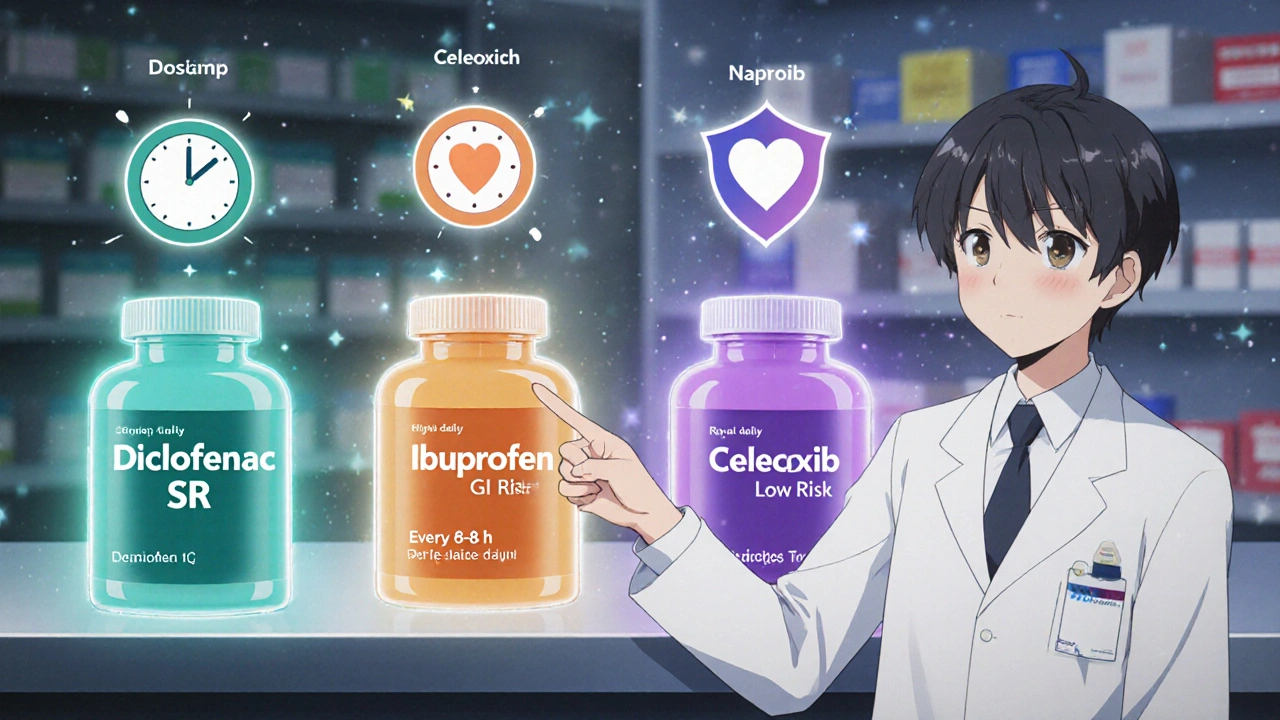
In everyday practice, naproxen tends to offer a longer half‑life, which means fewer doses per day and steadier pain control for conditions like osteoarthritis. Diclofenac, on the other hand, is often praised for its rapid onset, making it a go‑to for acute joint flare‑ups. The effectiveness‑duration trade‑off creates a semantic triple: naproxen provides sustained relief, while diclofenac delivers quick onset; together they encompass the full spectrum of pain management needs. Both drugs share the same COX‑inhibiting mechanism, but diclofenac’s stronger COX‑2 selectivity can translate into slightly higher cardiovascular considerations, linking the entity cardiovascular risk to drug selection. Meanwhile, naproxen’s milder impact on platelet function means it’s sometimes preferred for patients on low‑dose aspirin, illustrating how NSAIDs require individualized safety monitoring.
Beyond efficacy, dosage forms and availability shape the decision. Naproxen is available over the counter in 220 mg tablets, while diclofenac often requires a prescription, especially for the extended‑release or topical gels used in sports injuries. This availability difference feeds into the semantic connection: prescription status influences accessibility, which in turn affects adherence. Renal function is another piece of the puzzle—both drugs can reduce kidney blood flow, but diclofenac’s higher renal clearance demand makes it less suitable for patients with chronic kidney disease. This links the entity gastrointestinal side effects to broader renal safety concerns, reinforcing why physicians weigh multiple health factors before writing a script.
Putting it all together, the collection below dives deeper into each angle: dosage tips, side‑effect management, cost comparisons, and real‑patient experiences. Whether you’re a patient trying to pick the right pill, a caregiver sorting out medication schedules, or a health‑pro looking for a quick refresher, these articles give you actionable insights that go beyond the headline comparison. Explore the posts to see how naproxen vs diclofenac plays out across different conditions, ages, and health profiles.