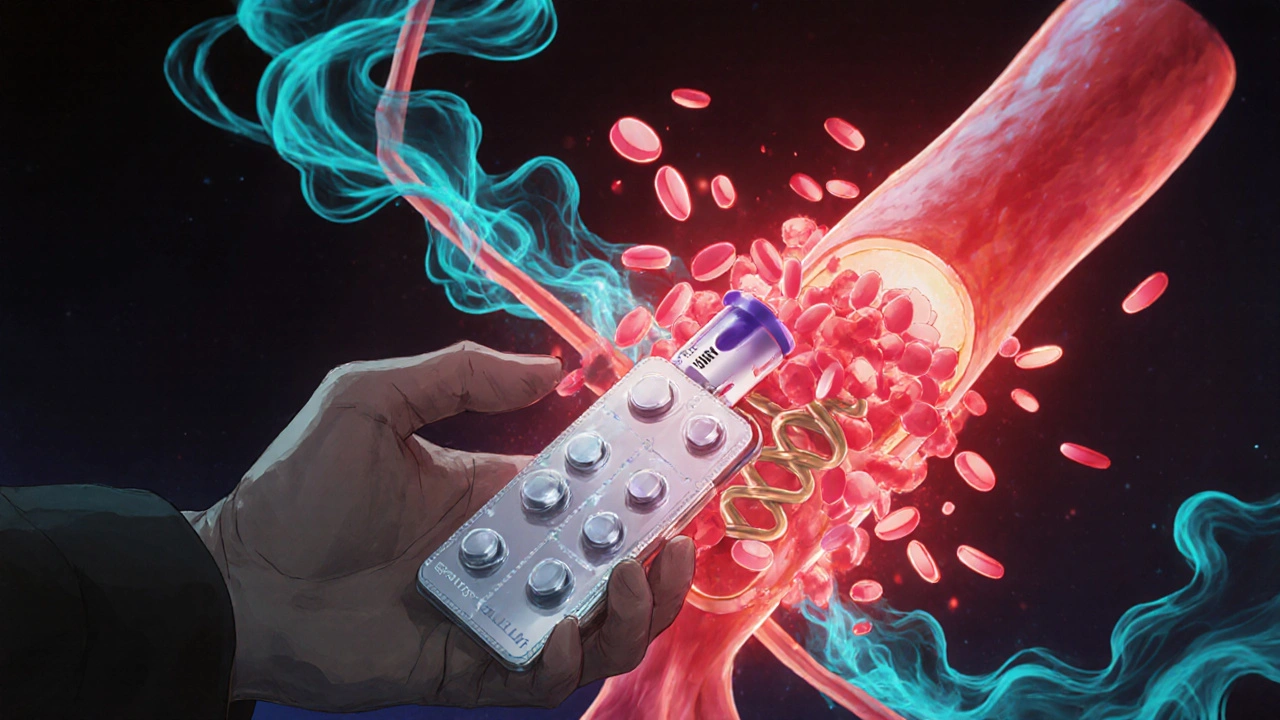
When your heart artery gets blocked by a clot, your body needs help preventing another one. That’s where dual antiplatelet therapy, a treatment combining two antiplatelet drugs to stop blood clots from forming. Also known as DAPT, it’s a standard approach after a heart attack, stent placement, or certain types of stroke. It’s not just one drug doing the work—it’s two working in sync to block different pathways that make platelets sticky. Without it, clots can form inside stents or arteries, leading to another heart attack or even death.
This therapy usually starts with aspirin, a common, low-cost drug that blocks a key enzyme in platelet activation, paired with another antiplatelet like clopidogrel, a stronger agent that targets a different receptor on platelets. Together, they’re more effective than either alone. But it’s not for everyone. Doctors weigh risks—like bleeding in the stomach or brain—against the benefit of preventing clots. Some patients need it for just a month after a stent. Others stay on it for a year or longer. Newer drugs like ticagrelor and prasugrel are also used, especially when clopidogrel doesn’t work well for certain people.
What you’ll find in this collection are real comparisons of these drugs, how they stack up against each other, and what happens when you switch or stop. You’ll see how aspirin works for clot prevention, why some people need to avoid it, and how alternatives like clopidogrel or newer agents compare in cost, side effects, and effectiveness. There’s also advice on managing bleeding risks, what to do if you miss a dose, and how lifestyle changes support the treatment. This isn’t theory—it’s what doctors and patients actually deal with every day.