When working with celecoxib, a selective COX‑2 inhibitor used to reduce inflammation and pain. Also known as Celebrex, it targets the cyclooxygenase‑2 enzyme while sparing COX‑1, which helps lower stomach irritation compared with traditional NSAIDs, non‑steroidal anti‑inflammatory drugs that block both COX‑1 and COX‑2. Because of this selective action, celecoxib is often chosen for chronic conditions like arthritis, joint inflammation that can limit mobility and cause daily pain, but it still carries a set of cardiovascular and gastrointestinal considerations.
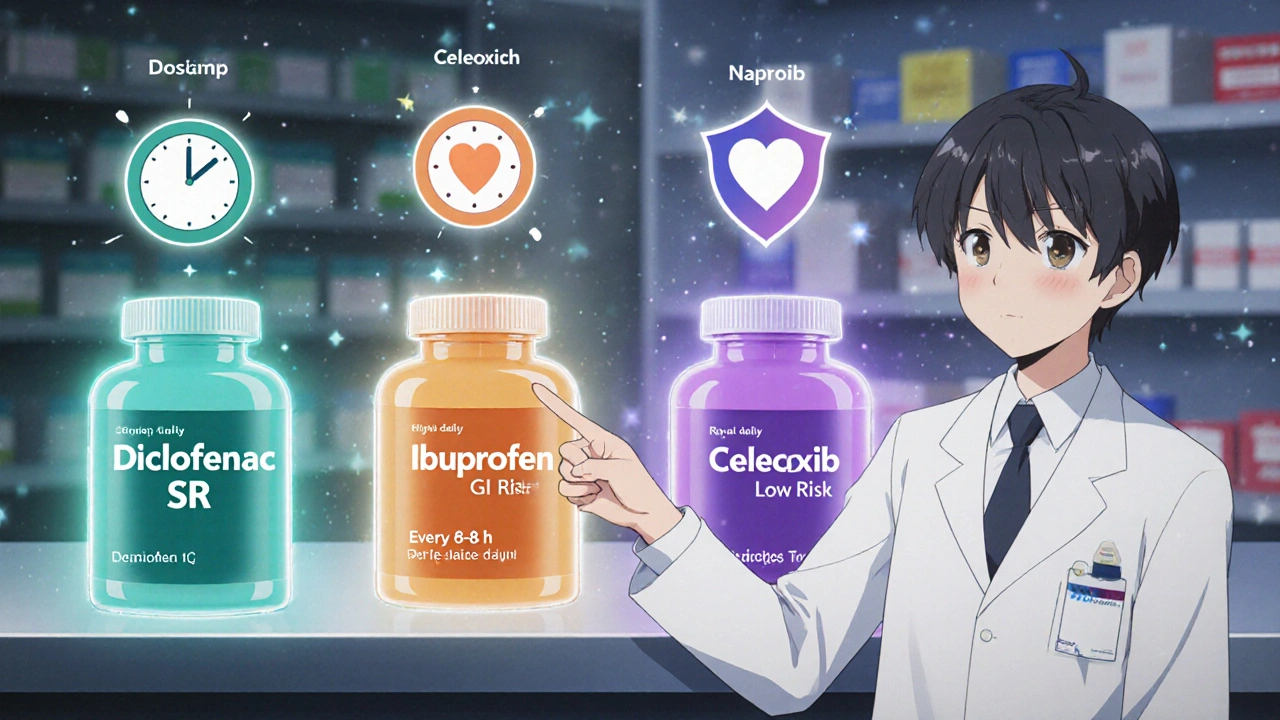
One of the biggest semantic connections here is that celecoxib encompasses the broader class of COX‑2 inhibitors, which were developed to improve the safety profile of older NSAIDs. This relationship means that anyone evaluating pain‑relief options should compare celecoxib against other COX‑2 agents like etoricoxib or traditional NSAIDs such as ibuprofen. While celecoxib reduces the risk of stomach ulcers, it can raise concerns about heart health, especially in patients with existing cardiovascular disease. In practice, clinicians often weigh the benefit‑risk ratio by checking blood pressure, cholesterol levels, and personal history of heart attacks before prescribing.
First, dosage matters. The typical range for osteoarthritis is 200 mg once daily, while rheumatoid arthritis may need 100‑200 mg twice daily. This dosing pattern influences how the drug is metabolized by the liver enzyme CYP2C9, which can interact with common medications like warfarin or certain antidepressants. Understanding this metabolic pathway helps avoid dangerous drug‑drug interactions. Second, timing of meals can affect absorption; taking celecoxib with food slows peak concentration but can improve tolerability for sensitive stomachs.
Third, patient age plays a role. Older adults often have reduced kidney function, so the drug’s renal clearance may be slower, increasing systemic exposure. In such cases, lower doses or alternative therapies are recommended. Fourth, the presence of risk factors like smoking, high blood pressure, or diabetes pushes the decision toward a more conservative approach, perhaps opting for topical NSAIDs instead of oral celecoxib.
Finally, monitoring is essential. Regular check‑ups should include blood pressure readings, lipid panels, and, if the patient is on anticoagulants, clotting tests. Any sign of new chest pain, shortness of breath, or swelling in the legs warrants immediate medical attention because those symptoms could signal a cardiovascular event linked to COX‑2 inhibition.
Beyond the clinical side, many users wonder how celecoxib stacks up against lifestyle changes. Exercise, weight management, and a diet rich in omega‑3 fatty acids can lower inflammation naturally, potentially allowing a lower drug dose. Supplements like turmeric or glucosamine may provide additive relief, but they should be discussed with a healthcare provider to avoid unexpected interactions.
In short, the celecoxib landscape is a balancing act between effective pain control and vigilant risk management. The posts you’ll find below dig into specific scenarios—such as switching from traditional NSAIDs, handling side‑effects, and combining celecoxib with other therapies—so you can make an informed choice that fits your health profile.
Ready to explore detailed comparisons, dosage guides, and safety tips? Scroll down to see the curated articles that break down celecoxib’s role in everyday medicine, from arthritis relief to cardiovascular considerations.