When talking about bone health, the condition of your skeleton’s strength, density, and ability to repair itself. Also known as skeletal health, it matters at any age because bones support movement, protect organs, and store minerals. As you get older, bone turnover shifts and loss can outpace formation, making nutrition and lifestyle choices critical. The right mix of weight‑bearing activity, balanced diet, and smart medication use can keep your bones resilient and reduce fracture risk.
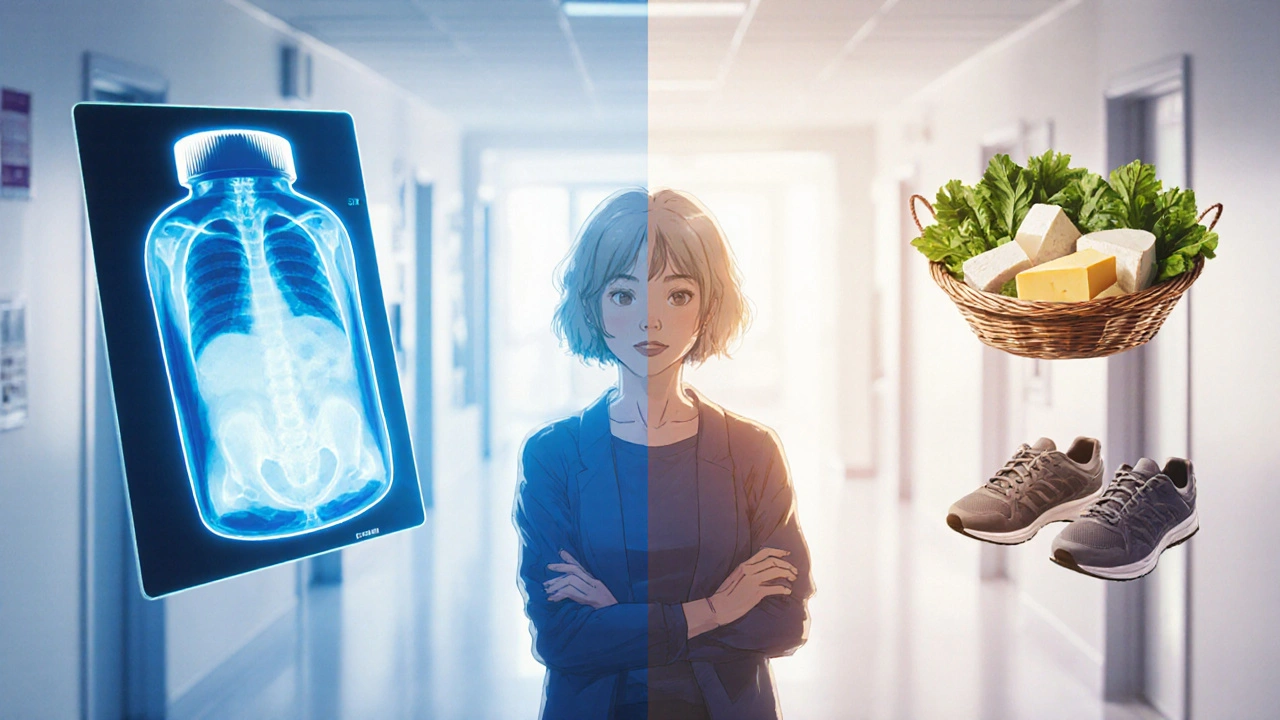
One of the most direct ways to boost bone health is through adequate mineral intake. Calcium, the primary mineral forming bone matrix is the foundation; without enough, bones become porous and fragile. Vitamin D, a fat‑soluble vitamin that enhances calcium absorption in the gut works hand‑in‑hand with calcium, ensuring the mineral actually reaches the bone tissue. Together they form a semantic triple: bone health encompasses calcium intake, calcium supports bone density, and vitamin D enhances calcium absorption. Food sources like dairy, leafy greens, fortified plant milks, and safe sunlight exposure cover most needs, but many adults benefit from supplements, especially in winter months or when dietary restrictions apply.
Beyond minerals, protein and other micronutrients play supporting roles. Adequate protein supplies the building blocks for the collagen scaffold that holds calcium crystals, while magnesium and vitamin K2 help regulate bone remodeling. Regular resistance training—think squats, push‑ups, or even brisk walking—creates micro‑stress that signals the body to lay down fresh bone tissue, further reinforcing the mineral framework.
When the balance tips toward loss, diseases like Osteoporosis, a condition marked by reduced bone mass and structural deterioration become a major concern. Osteoporosis threatens bone health by increasing fracture susceptibility, especially in the hip, spine, and wrist. Several medication classes either help or harm this balance. Bisphosphonates, drugs that slow bone resorption by inhibiting osteoclast activity are the go‑to treatment for many patients, effectively reducing fracture rates. On the flip side, long‑term use of glucocorticoids like prednisolone can trigger bone loss, making steroid‑induced osteoporosis a real risk. Even common over‑the‑counter choices such as aspirin, when taken in high doses for extended periods, may subtly affect platelet function and micro‑circulation around bone tissue, influencing healing after injury.
Understanding how each drug interacts with bone metabolism lets you make smarter choices with your doctor. For example, pairing a bisphosphonate regimen with calcium and vitamin D supplementation maximizes benefit, while monitoring bone density scans can catch early signs of medication‑related decline. Lifestyle tweaks—reducing excess alcohol, quitting smoking, and staying active—complement pharmacologic strategies and keep the skeletal system robust.
Below you’ll find a curated list of articles covering the medications, nutrients, and conditions that intersect with bone health. From detailed guides on aspirin’s role in embolism prevention to practical tips for managing prednisolone‑induced acne (a side effect that can hint at steroid‑related bone issues), each piece adds a layer of insight. Dive in to see how these topics connect to keeping your skeleton strong, and use the information to discuss personalized plans with your healthcare provider.