When your pharmacist hands you a pill that looks nothing like the one you’ve been taking for years, it’s normal to feel uneasy. The shape is different. The color is off. The name on the tablet isn’t the one your doctor wrote. This is generic substitution - and it’s happening more often than you think. In the U.S., generic drugs now make up about 90% of all prescriptions filled. That’s not just a trend - it’s policy, economics, and everyday healthcare in action.
Why Are You Being Switched?
The short answer: money. Brand-name drugs can cost hundreds or even thousands of dollars a month. Generics? Often under $20. Insurance companies push generics because they save billions. The FDA estimates that generic drugs saved the U.S. healthcare system $370 billion in 2023 alone. That’s not a rounding error - it’s life-changing for people who can’t afford their meds. But here’s the catch: switching isn’t always as simple as swapping one pill for another. Some people experience real changes in how they feel after the switch. Others notice nothing at all. Why the difference?Are Generics Really the Same?
The FDA says yes. By law, a generic drug must have the same active ingredient, strength, dosage form, and route of administration as the brand-name version. It must also be bioequivalent - meaning it gets into your bloodstream at the same rate and to the same extent. The acceptable range for bioequivalence is 80% to 125% of the brand’s performance. That’s tight. That’s regulated. So why do some patients report problems? The answer lies in what’s not in the label: the inactive ingredients. Fillers, dyes, preservatives, coatings - these vary between manufacturers. For most people, they’re harmless. But for some, especially those with sensitivities, they can cause side effects like stomach upset, rashes, or even changes in how the drug is absorbed.Where Switching Gets Tricky
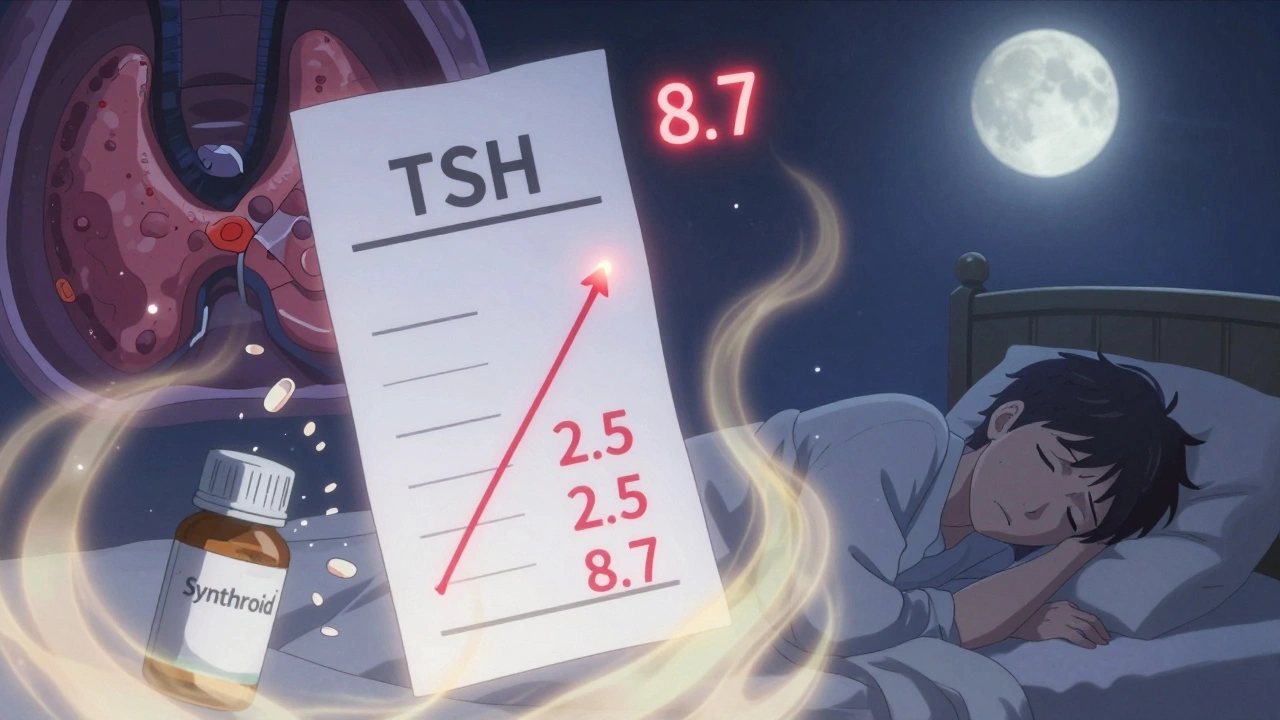
Not all drugs are created equal when it comes to switching. Some have a narrow therapeutic index - meaning even tiny changes in blood levels can cause big problems. These include:- Levothyroxine (for hypothyroidism): Small changes in thyroid hormone levels can throw off your metabolism, heart rate, and energy. Patients switching from Synthroid to generic levothyroxine have reported TSH levels jumping from 2.5 to 8.7 in just six weeks - a clear sign the dose isn’t working the same.
- Warfarin (a blood thinner): Even slight variations in concentration can lead to dangerous clots or bleeding. Many doctors avoid switching patients on warfarin unless absolutely necessary.
- Anti-seizure medications (like phenytoin or carbamazepine): Multiple studies show increased seizure frequency after switching to generics. One review found that patients with epilepsy were more likely to have breakthrough seizures after a generic switch.
What You Might Notice After Switching
People report a range of experiences:- Nothing changes. Most patients - about 78% according to Drugs.com reviews - say generics work just as well. They save money. They feel fine.
- They feel worse. Fatigue, headaches, mood swings, or worsening symptoms. This is often tied to the inactive ingredients or inconsistent absorption.
- The pill looks different every time. Because generics come from different manufacturers, your pill might be blue one month, white the next, oval instead of round. This causes confusion. One Massachusetts patient survey found 63% of people were initially worried about efficacy - but 82% were satisfied after three months.
How to Protect Yourself
You don’t have to accept a switch blindly. Here’s what to do:- Ask your doctor - “Can I stay on the brand name?” If you’ve been stable on a brand drug for years, especially with a narrow therapeutic index, your doctor can write “dispense as written” or “do not substitute” on the prescription.
- Check the label - If the pill looks different, call your pharmacy. Ask if the manufacturer changed. Ask for the name of the generic maker. Some pharmacies now label vials with the manufacturer’s name to help you track changes.
- Monitor your symptoms - Keep a simple log: date, pill appearance, how you feel. If you notice changes in energy, mood, heart rate, or seizure frequency, document it.
- Don’t panic, but don’t ignore it - If you feel off after a switch, don’t assume it’s “all in your head.” Go back to your doctor. Bring your log. Ask if switching back is an option.
- Know your insurance - Many plans won’t cover brand-name drugs unless you’ve tried and failed the generic. But if you’ve had a bad reaction, you can appeal. Many insurers will approve the brand if you have documentation.
Why Do Generics Look Different?
It’s not a trick. It’s the law. Trademark rules prevent generic manufacturers from copying the exact shape, color, or imprint of brand-name pills. That’s why your Xanax might be a white oval one month and a blue capsule the next. It’s the same active ingredient - alprazolam - but a different manufacturer, different fillers, different coating. Some pharmacies now use stickers or inserts to warn you when the pill has changed. Others don’t. That’s why asking questions matters.What About Recalls?
You’ve probably heard about recalls - especially for generics made overseas. That’s real. But here’s the truth: brand-name drugs are made overseas too. The FDA inspects all facilities, regardless of origin. A recall doesn’t mean the drug is unsafe - it means a manufacturing issue (like a foreign particle or wrong label) was found. It’s not unique to generics. Still, if you’re worried, ask your pharmacist: “Where is this made?” and “Has this batch been recalled?”
When Switching Is a Good Idea
For many drugs - antibiotics, statins, blood pressure meds, antidepressants - switching to generic is safe, effective, and smart. Studies show no difference in outcomes for these drugs. The cost savings are huge. And for people who couldn’t afford their meds before, generics mean they actually take them. A 2019 report found that brand-name drugs had 266% higher abandonment rates than generics. That means people just stopped taking them because they were too expensive. Generics saved lives.What’s Changing Now?
Some states, like Massachusetts, require pharmacists to substitute generics unless the doctor says no. Other states leave it up to the pharmacist. That inconsistency adds confusion. Meanwhile, health systems are starting to notice the problem with too-frequent switching. In Saudi Arabia, over 25% of medications changed between brand and generic versions in just five years because of annual government bidding. That meant patients got a different generic every few months - and with it, more confusion and errors. Experts now recommend: stick with one generic manufacturer if possible. If your pharmacy switches you every refill, ask if they can get you the same one consistently.The Bottom Line
Generic drugs are not inferior. They’re not cheap knockoffs. They’re rigorously tested, FDA-approved, and effective for most people. But they’re not always identical in how your body responds - especially for drugs where small changes matter. Your health isn’t a commodity. You have the right to ask questions. You have the right to say no. You have the right to speak up if something feels off. If you’ve been stable on a brand drug for years, don’t assume you need to switch. If you’re on a high-risk medication like levothyroxine or warfarin, talk to your doctor before accepting a generic. If you’re switching and feel worse - don’t wait. Document it. Go back. Ask for help. Saving money matters. But so does feeling well.Are generic drugs as effective as brand-name drugs?
For most drugs, yes. The FDA requires generics to be bioequivalent to brand-name versions, meaning they deliver the same amount of active ingredient at the same rate. Studies show no difference in effectiveness for antibiotics, statins, blood pressure meds, and many others. But for drugs with a narrow therapeutic index - like levothyroxine, warfarin, or anti-seizure medications - even small differences in absorption can cause noticeable changes in how you feel. Some patients report worsening symptoms after switching, even though the active ingredient is the same.
Why do generic pills look different?
Trademark laws prevent generic manufacturers from copying the exact shape, color, or imprint of brand-name pills. So even though the active ingredient is identical, the pill might be a different color, size, or shape. This is legal and intentional - not a sign of lower quality. But it can confuse patients, especially if the pill changes every time they refill. Some pharmacies now label vials with the manufacturer’s name to help track these changes.
Can I ask my doctor to keep me on the brand-name drug?
Yes. Your doctor can write “dispense as written” or “do not substitute” on your prescription. This tells the pharmacy not to switch you to a generic. This is especially important if you’re on a drug with a narrow therapeutic index, like levothyroxine, warfarin, or anti-seizure medications. Many insurance plans require you to try the generic first, but if you’ve had a bad reaction, you can appeal and provide documentation.
What should I do if I feel worse after switching to a generic?
Don’t ignore it. Keep a simple log: note the date you switched, what the pill looked like, and how you’re feeling - fatigue, mood changes, heart palpitations, seizures, etc. Bring this to your doctor. Ask if the switch could be causing the issue. In many cases, switching back to the brand or sticking with one generic manufacturer can resolve the problem. For drugs like thyroid medication or blood thinners, even small changes can have big effects.
Are generic drugs made in the same places as brand-name drugs?
Yes. Many brand-name drugs are manufactured overseas, and so are generics. The FDA inspects all facilities - whether they make brand or generic drugs - and requires them to meet the same quality standards. Recalls happen for both types, usually due to labeling errors or foreign particles, not because the active ingredient is weak. Don’t assume generics are riskier just because they’re cheaper. The issue isn’t origin - it’s consistency.
Why do some pharmacies switch me to a different generic every time?
It’s often due to pricing. Pharmacies buy from the lowest-cost supplier, which changes frequently. In some states, insurance contracts require them to use the cheapest option available. This means you might get one generic this month, a different one next month - even if you’ve been stable. Ask your pharmacy if they can get you the same manufacturer consistently. Some patients benefit from sticking with one version to avoid confusion or absorption changes.



15 Comments
kevin moranga December 12, 2025 AT 23:51
Hey, I’ve been on generic levothyroxine for three years now and honestly? I feel better than ever. My TSH stayed stable, my energy’s up, and I’m saving like $120 a month. I get why people worry-my mom freaked out when her pills changed color-but sometimes the fear’s worse than the switch. Give it a real shot before you go back. Your wallet (and your thyroid) will thank you. 😊
Lara Tobin December 14, 2025 AT 19:20
I switched to generic warfarin last year and started bruising like a toddler on a trampoline. I didn’t say anything at first because I thought I was just ‘being dramatic.’ But when I started getting nosebleeds every morning, I finally brought my log to my doctor. Turns out, my INR spiked. We switched back. I’m not ‘overreacting’-I’m alive. 🙏
Scott Butler December 15, 2025 AT 07:52
Anyone who says generics are ‘just as good’ hasn’t lived in the real world. The FDA’s standards are a joke. I’ve had generics made in India that looked like they were pressed by a toddler with a Play-Doh set. And now you want me to trust that? We’re outsourcing our health to the lowest bidder and calling it ‘progress.’ Wake up.
Deborah Andrich December 15, 2025 AT 17:44
I’m a nurse and I’ve seen this over and over. People panic when the pill changes color. Then they stop taking it. Then they end up in the ER. The real problem isn’t the generic-it’s the lack of communication. Pharmacies need to hand you a slip that says ‘New maker: Teva. Same active ingredient.’ Simple. Human. We’re failing patients by treating them like robots.
Himmat Singh December 16, 2025 AT 00:08
It is a demonstrable fact that the FDA's bioequivalence standards are statistically insufficient to guarantee therapeutic equivalence across all patient populations. The 80%-125% confidence interval, while mathematically elegant, ignores inter-individual pharmacokinetic variance, particularly in elderly, renally impaired, or polypharmacological cohorts. To assert uniform efficacy is not merely misleading-it is a systemic epistemological failure of regulatory science.
Richard Ayres December 16, 2025 AT 13:29
Interesting post. I’ve been on generic statins for seven years. No issues. But I also know someone who had breakthrough seizures after switching from brand to generic carbamazepine. So I get the concern. I think the key is knowing your drug class. For most things? Generic’s fine. For narrow TI meds? Ask for the brand-or stick with one generic maker and never switch again. Consistency beats cost every time.
Sheldon Bird December 17, 2025 AT 06:40
My dad’s on levothyroxine and switched to generic last year. He was tired all the time, gained weight, couldn’t focus. We called the pharmacy and found out they switched him from Mylan to Teva without telling him. We went back to Mylan-same generic, different maker-and boom, he’s back to his old self. So it’s not always ‘brand vs generic’-it’s ‘which generic?’ 😊
Karen Mccullouch December 18, 2025 AT 23:02
Of course generics are dangerous. Why do you think the FDA lets them be made in China? We’re letting foreign factories cut corners on our medicine while our own factories sit empty. This isn’t ‘savings’-it’s national surrender. My cousin’s mom died because her generic blood pressure med didn’t work right. Don’t tell me it’s ‘the same.’ It’s not. It’s cheaper. Big difference.
Michael Gardner December 20, 2025 AT 03:56
So you’re telling me the FDA says generics are bioequivalent, but then you list all these drugs where people have problems? That’s not a contradiction-it’s a confession. If the system’s so perfect, why do people need to log their pill colors and scream at their pharmacists just to stay alive? The answer’s obvious: the system doesn’t care. It just wants you to shut up and take the $3 pill.
John Fred December 21, 2025 AT 01:25
Just had a 72-year-old patient on generic levothyroxine come in with TSH of 14.2. She was confused, cold, and couldn’t walk without help. Switched back to Synthroid-7 days later, she’s hiking again. 💪 The FDA says ‘bioequivalent’ but your body doesn’t read the label. It feels the difference. Always ask: ‘Is this the same maker as last time?’ If not, push back. Your life > their profit margin. 📉💊
Hamza Laassili December 22, 2025 AT 14:07
generic drugs r not even real drugs!! they r just chemicals in a pill!! how can you trust somethin that looks diff every time?? i mean come on!! the brand name is the only thing that matters!! i dont care if it costs 300 bucks!! i want the real thing!!
Rawlson King December 24, 2025 AT 12:26
Anyone who claims generics are ‘just as good’ has never had to take a drug that requires precise dosing. This is not a debate about cost-it’s about clinical competence. If you can’t replicate bioavailability within a 5% margin, you don’t deserve to be called a pharmaceutical. The current system is a failure of regulatory oversight, not a triumph of efficiency.
Cole Newman December 25, 2025 AT 09:21
Wait so you’re telling me I can’t just trust my pharmacist? I thought they were the experts. Now I have to keep a journal of my pill colors? And call my doctor every time it changes? What am I, a scientist? I just want to feel better. This is too much work. Can’t someone just fix this?
Casey Mellish December 25, 2025 AT 23:21
As an Aussie, I’ve been on generics for everything since I was 18. No issues. But I do get why Americans are stressed-your system is a mess. Here, the government negotiates prices and picks one generic manufacturer per drug nationwide. You get the same pill every time. No confusion. No panic. Just medicine. Maybe the problem isn’t generics-it’s the chaotic, profit-driven mess you call healthcare.
Tyrone Marshall December 27, 2025 AT 17:26
There’s a deeper question here: why do we treat medicine like a commodity? We don’t do this with airplane parts or heart valves. We demand precision, consistency, accountability. But for pills? We accept color changes, manufacturer roulette, and silent substitutions. Maybe the real issue isn’t whether generics work-it’s whether we’ve lost the moral courage to demand better for our bodies. You deserve more than a lottery ticket with your prescription.