Every year, more than 5.8 billion prescription drug packages move through the U.S. supply chain-from factories to warehouses, pharmacies, and finally to patients. Behind that number is a hidden battle: protecting real medicine from fake. Counterfeit drugs don’t just waste money. They can kill. A pill with the wrong ingredient, the wrong dose, or no active drug at all can turn a life-saving treatment into a death sentence. So how do we make sure the medicine you pick up at the pharmacy is the real thing? The answer isn’t just better security cameras or stricter laws. It’s a complex, high-tech system built over a decade, called the Drug Supply Chain Security Act (DSCSA).
The DSCSA: The Backbone of Drug Safety
The DSCSA, signed into law in 2013, didn’t just add another rule. It rewrote how drugs are tracked from the moment they leave the factory until they’re handed to you. Before DSCSA, tracing a drug back to its source could take weeks. Today, it takes seconds. The law forces every player in the chain-manufacturers, wholesalers, repackagers, and pharmacies-to use unique digital identifiers on every single package. That’s not just a barcode. It’s a digital fingerprint: a 2D Data Matrix code that holds the National Drug Code (NDC), a serial number, the lot number, and the expiration date. Each package gets its own unique code. Every day, over 1.2 million of these codes are generated across the U.S.How Serialization Works in Practice
Imagine a bottle of blood pressure medication. At the factory, each bottle gets a serial number stamped onto its label. That number isn’t reused. It’s stored in a secure database linked to the manufacturer. When the drug moves to a wholesaler, the barcode is scanned. The system checks: Is this serial number real? Is it from an authorized supplier? Is it still within its expiration window? If anything looks off, the system flags it. That’s serialization-making every package uniquely identifiable. But serialization alone isn’t enough. That’s where traceability comes in. Every time the drug changes hands, the transaction details-what was shipped, when, and from whom-are recorded electronically. No more paper logs. No more hand-written receipts. Everything is stored in a standardized digital format called EPCIS, developed by GS1. This system handles over 15 million transactions daily with 99.95% accuracy. If a fake drug slips into the system, regulators can trace it back to the exact warehouse, truck, or pharmacy that handled it-within hours, not days.Verification: Catching Fakes Before They Reach You
The system doesn’t just track. It verifies. Every pharmacy and hospital must check the serial number of any drug they receive against the manufacturer’s database. If the number doesn’t match-or if it’s been used before-the system rejects it. This isn’t theoretical. In 2022, the FDA reported 412 counterfeit drug seizures. That’s down from 1,103 in 2014. That 63% drop didn’t happen by accident. It happened because pharmacies and distributors now have tools to spot fakes in real time. The verification process is automated. When a pharmacist scans a bottle, the system sends the serial number to the manufacturer’s server. If the manufacturer says, “Yes, this is real,” the drug moves forward. If the server says, “This number was reported stolen,” or “This product was never made,” the system locks it out. In one case, a small pharmacy in Ohio caught three fake insulin vials because their system flagged the serial numbers as invalid. The drugs were quarantined. No one was harmed.
Authorized Trading Partners: Who’s Allowed in the Chain?
Not everyone gets to handle prescription drugs. The DSCSA requires every company in the supply chain to be verified as an Authorized Trading Partner (ATP). That means the FDA checks their credentials, licenses, and compliance history before they’re allowed to trade. The FDA’s ATP Verification Router Service handles over 50,000 of these checks every day, with a 99.8% success rate. If a company isn’t on the list, their drugs can’t be legally sold. This stops shady operators from slipping in. In 2021, a company in Florida tried to sell bulk batches of metformin to a distributor. The distributor scanned the serial numbers and found they weren’t registered with the manufacturer. The FDA was notified. The shipment was seized. The company was shut down. Without ATP verification, that fake drug could have ended up in a patient’s medicine cabinet.International Differences: Why the U.S. System Is Unique
The U.S. doesn’t have the only drug safety system. The European Union uses the Falsified Medicines Directive (FMD). It’s similar but different. The EU requires all prescription drugs to have an anti-tamper seal and a unique code. But instead of a decentralized network like the U.S., the EU uses a centralized database where every pharmacy must connect to a national verification system. When a pharmacist scans a pill, it’s checked against a single EU-wide repository. The U.S. system is more flexible. It lets companies choose their own software platforms, as long as they follow EPCIS standards. That’s why companies like TraceLink, SAP, and Movilitas dominate the U.S. market-they build the software that connects manufacturers to pharmacies. The EU system is more uniform but harder to scale. The U.S. approach allows innovation but creates complexity. A global drug company must run two different systems-one for the U.S., one for Europe-increasing compliance costs by 22%, according to PwC.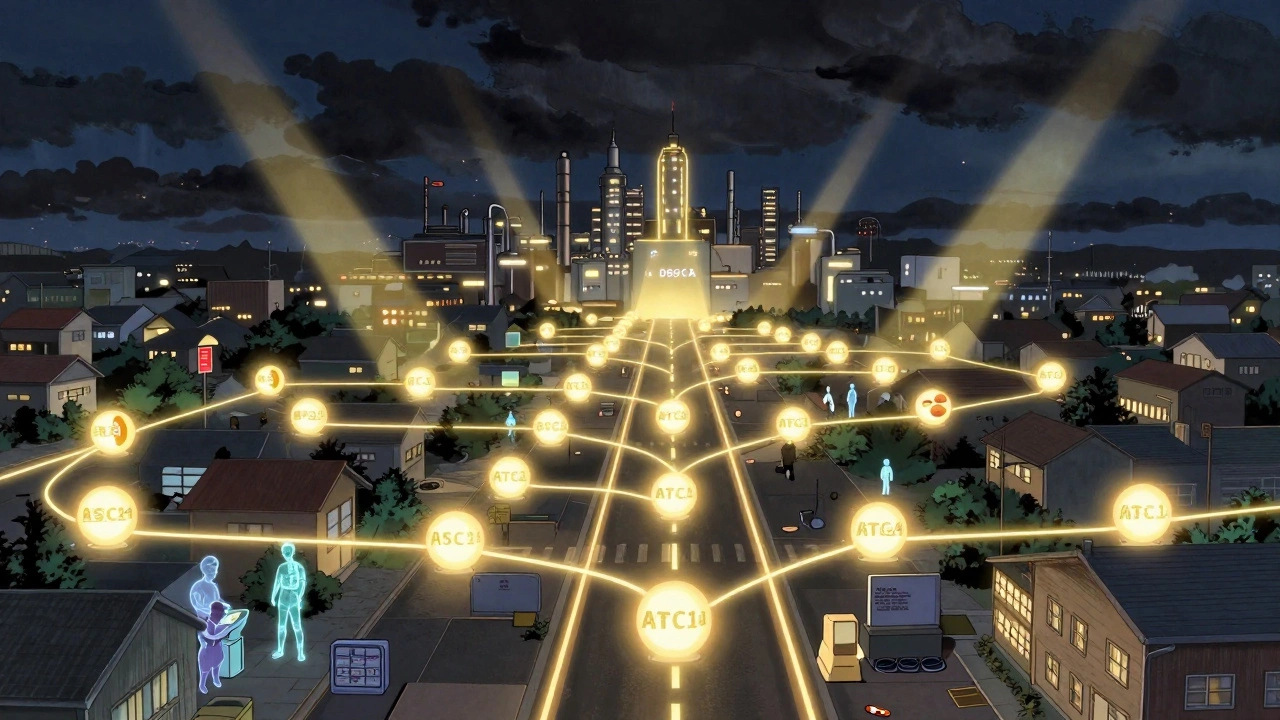
Challenges: Where the System Still Has Gaps
No system is perfect. One big weakness is repackaging. When a hospital takes a bulk bottle of pills and puts them into smaller blister packs, the original barcode is destroyed. That means the new pack doesn’t have the original serial number. The FDA allows this, but it creates a blind spot. The repackaged drug is still tracked, but not with the same level of detail. Experts warn this is where counterfeiters might try to sneak in fake drugs disguised as repackaged products. Another issue is integration. Many small pharmacies still use old computer systems that weren’t built for high-speed barcode scanning or digital data exchange. A 2023 survey found that 63% of independent pharmacies with fewer than 10 employees struggled to meet the 2023 electronic data requirements. One pharmacy owner in Oregon told a trade journal he spends $18,500 a year just on DSCSA software and scanners-3.2% of his net profit. For a small business, that’s a heavy burden. Cybersecurity is another concern. In early 2023, a major healthcare IT company was hacked. For 72 hours, pharmacies couldn’t verify drug serial numbers. That’s a huge risk. If the verification system goes down, fake drugs could slip through. The FDA has since pushed for backup protocols, but many smaller providers still lack them.What’s Next? The Road to 2027
The DSCSA isn’t finished. The final deadline is November 2027. By then, every single drug transaction must happen electronically. No paper. No fax. No manual entry. Everything must be exchanged in a standardized, interoperable format. Right now, 14% of transactions still use paper. That’s changing fast. The FDA’s 2023 guidance now requires all systems to use EPCIS 2.0 with JSON format by November 2025. That’s a major shift-most companies are still using older XML systems. The goal? A fully connected, real-time drug tracking network. Imagine if your pharmacist could instantly tell you not just if your drug is real, but where it was made, when it was shipped, and whether it stayed within temperature limits during transport. That’s coming. Some companies are already testing blockchain for drug tracking. Others are using AI to spot unusual patterns-like a sudden spike in requests for a specific drug in one region, which could signal a counterfeit ring.Why This Matters to You
You might think, “I don’t work in pharma. Why should I care?” But here’s the truth: the system protecting your medicine is the same one that protects your parent’s insulin, your child’s antibiotics, or your grandparent’s heart medication. When that system works, you get the right drug. When it fails, people die. The DSCSA has already prevented thousands of fake drugs from reaching patients. It’s not perfect. It’s expensive. But it’s working. The next time you pick up a prescription, look at the packaging. That tiny barcode isn’t just for scanning. It’s your safety net. It’s the result of billions of dollars in investment, thousands of hours of coding, and a decade of regulatory effort. It’s the reason you can trust that what you’re taking will help you-not hurt you.How does the DSCSA prevent counterfeit drugs from entering the U.S. supply chain?
The DSCSA prevents counterfeit drugs by requiring every prescription drug package to have a unique digital identifier (serial number) embedded in a 2D barcode. Every time the drug changes hands, the transaction is recorded electronically using standardized EPCIS format. Pharmacies and distributors must verify each serial number against the manufacturer’s database before dispensing. If a number is invalid, stolen, or duplicated, the system blocks the product. This creates a chain of accountability that makes it nearly impossible for fake drugs to move undetected.
What happens if a pharmacy finds a suspect drug?
If a pharmacy or distributor finds a suspect drug-whether the barcode doesn’t scan, the serial number is invalid, or the product looks tampered with-they must immediately quarantine it. They’re required to notify the manufacturer and the FDA within 24 hours. The manufacturer then investigates: Is this a real product? Was it stolen? Was it repackaged illegally? If confirmed as fake, the FDA issues a recall, and the drug is destroyed. In 2022, this process stopped over 12,000 suspect products from reaching patients.
Are all drugs in the U.S. required to have serial numbers?
Only prescription drugs are required to have serialized barcodes under the DSCSA. Over-the-counter (OTC) medications, dietary supplements, and biological products like vaccines are not currently covered by the same rules. However, many vaccine manufacturers voluntarily use serialization for tracking, especially after the success of the COVID-19 vaccine distribution. The FDA has considered expanding serialization to OTC drugs, but no timeline has been set.
How do I know if the medicine I’m taking is real?
As a patient, you don’t need to check the barcode yourself. The system does it for you. But you can protect yourself by only getting prescriptions filled at licensed pharmacies-never from online sellers without a physical address or a licensed pharmacist on staff. If your medication looks different than usual-different color, shape, or packaging-ask your pharmacist. They’re trained to spot anomalies. The DSCSA ensures your pharmacist can verify the drug’s authenticity before giving it to you.
Is the DSCSA system foolproof?
No system is foolproof. The DSCSA has dramatically reduced counterfeit drugs, but gaps remain. Repackaged drugs lose their original serial numbers, creating vulnerabilities. Smaller pharmacies still struggle with tech costs and integration. Cyberattacks can temporarily disable verification systems. And international shipments-especially from countries without strong tracking rules-can slip through. But the system’s strength is speed: when a problem is found, it’s contained fast. That’s what saves lives.



9 Comments
Wendy Chiridza December 3, 2025 AT 11:46
The DSCSA is one of those quiet miracles that keeps us all safe without us even noticing. Every time I pick up my blood pressure pills, I think about that barcode and how it’s tied to a global system designed to catch fakes before they reach me. It’s not glamorous, but it’s vital. The fact that 99.95% of transactions are accurate? That’s engineering done right.
Pamela Mae Ibabao December 3, 2025 AT 14:03
Let’s be real-this whole system is overengineered. You’re telling me a small pharmacy in rural Oregon spends nearly 4% of their profit just to scan barcodes? Meanwhile, the FDA still lets repackaged drugs slide without full serialization. That’s not safety, that’s bureaucracy with a tech veneer. And don’t get me started on how the EU’s centralized system is actually more secure. But hey, at least we’ve got a cool infographic to show at cocktail parties.
Gerald Nauschnegg December 4, 2025 AT 04:09
Wait, so if I’m a pharmacist and my system goes down for 72 hours because of a hack, what happens? Do we just hand out meds like it’s 1998? I mean, I get the tech, but what’s the backup? Paper logs? That’s insane. I’ve seen pharmacies in my town use Excel sheets to track inventory. If this system crashes, we’re one bad actor away from a national crisis. Someone needs to audit the fail-safes. Like, yesterday.
Palanivelu Sivanathan December 6, 2025 AT 01:15
Ohhhhhhh... so this is what they mean by 'digital destiny'? Every pill, every bottle, every serial number-tracked like a soul in the machine? It’s beautiful, isn’t it? The modern pharmacy is now a temple of data, where the barcode is the holy glyph and the EPCIS protocol, the sacred chant. And yet... who watches the watchers? Who codes the code? Who ensures the manufacturer’s server doesn’t lie? The truth is, we’ve traded faith in medicine for faith in servers. And servers... can be hacked. Can be corrupted. Can be owned. The real counterfeit isn’t in the pill-it’s in the illusion of control.
Joanne Rencher December 6, 2025 AT 22:38
So we spend billions to scan barcodes but still let OTC meds slide? That’s like locking your front door but leaving the back window wide open. And why are we even talking about this like it’s a win? It’s not. It’s a band-aid on a bullet wound. The real problem? Profit-driven pharma and lazy regulators. This isn’t safety-it’s damage control with a fancy acronym.
Erik van Hees December 8, 2025 AT 07:09
Actually, you’re all missing the bigger picture. The DSCSA’s real innovation isn’t serialization-it’s the ATP verification system. That’s what stops the bad actors at the gate. The FDA’s database checks over 50k companies daily. That’s not just tech, that’s institutional muscle. And the fact that counterfeit seizures dropped 63%? That’s not luck. That’s enforcement. The system’s not perfect, but it’s the most effective drug safety net ever built. Stop complaining and appreciate the infrastructure.
Cristy Magdalena December 9, 2025 AT 00:17
I just read that a pharmacy in Ohio caught three fake insulin vials. Three. Three lives were saved because of a barcode. And I cried. Not because it’s impressive-it’s terrifying. That we have to rely on a digital fingerprint on a pill to keep someone from dying… that’s not progress. That’s a society that’s one server crash away from mass death. I’m not grateful. I’m terrified. And I’m not alone.
Adrianna Alfano December 9, 2025 AT 09:59
My grandma takes insulin too. She’s 82. Last month she said her pills looked different-paler, weird texture. I took her to the pharmacy and they scanned it. Turned out it was a new batch. But if it hadn’t been? I don’t even want to think about it. This system? It’s not just tech. It’s love in code. The fact that a small pharmacy in Oregon can afford this? They shouldn’t have to. But hey-at least it works. We need to fund these places, not just talk about how ‘complex’ it is.
Casey Lyn Keller December 10, 2025 AT 17:50
So the FDA says the system works. But what if the manufacturers are in on it? What if the databases are compromised? What if the whole thing’s just a distraction while the real counterfeit drugs come in through international mail? I’ve seen those packages. No barcode. No trace. Just a guy in a van with a suitcase full of fake pills. This whole thing feels like a magic show-look over there while they slip the real stuff through the back door.