Every year, over a million children under six in the U.S. are exposed to medications they weren’t supposed to take. Most of these cases aren’t accidents - they’re preventable. A child finds a bottle of pills on the nightstand, grabs a handful of gummy vitamins that look like candy, or gets confused when Mom gives them Tylenol for fever and Dad gives them a cold medicine that also has Tylenol. The result? A medical emergency that can turn deadly in minutes - or hours - without quick action.
What Does a Medication Overdose Look Like in a Child?
There’s no single sign of overdose. It depends on what the child took - and how much.For opioids like oxycodone, hydrocodone, or fentanyl, watch for these six clear signs:
- Pinpoint pupils - so small they look like dots
- Limp body, like a ragdoll
- Unresponsive, even when you shake them or shout
- Gurgling or choking sounds - like they’re drowning
- Slow, shallow, or stopped breathing
- Cold, clammy skin with blue or purple lips and fingernails
Acetaminophen (Tylenol) Overdose: The Silent Killer
Acetaminophen is the most common cause of pediatric poisoning. Why? Because it’s in so many things. Cold medicine. Pain relievers. Flu remedies. Even some prescription antibiotics. Parents think they’re being careful - until they give two products with the same active ingredient. Here’s the scary part: acetaminophen overdose often shows no symptoms for 24 hours. The child might seem fine. No vomiting. No crying. No fever. But inside their liver, damage is already spreading. By the time nausea, vomiting, or stomach pain shows up, it’s often too late for easy treatment. The Cleveland Clinic says N-acetylcysteine (NAC), the antidote for acetaminophen poisoning, is 100% effective if given within 8 hours. After 16 hours, it drops to 40%. That’s why you can’t wait for symptoms. If you suspect your child swallowed too much Tylenol - even if they seem okay - call Poison Control right away.Stimulant Overdose: ADHD Medications Gone Wrong
Children on ADHD meds like Adderall, Ritalin, or Vyvanse are at risk too. Overdose can happen if a child takes more than prescribed, or if someone else’s pills get mixed in. Signs include:- Extreme irritability or panic
- Rapid breathing or heart rate
- High fever
- Confusion, hallucinations, or seizures
- Blurred vision or chest pain
- Uncontrollable shaking

When to Call Poison Control - and When to Call 911
This is the most important thing to know: Call Poison Control at 800-222-1222 for any suspected overdose - even if your child seems fine. You don’t need to be sure. You don’t need to wait. Just call. Poison Control doesn’t just give advice. They connect you with real toxicologists who know exactly what to do based on the drug, the dose, and your child’s weight. They’ll tell you whether to watch, when to go to the ER, or if you need to give naloxone. But here’s the split-second decision: Call 911 if your child is:- Unresponsive - won’t wake up, even with loud noise or shaking
- Not breathing or breathing very slowly
- Having seizures or uncontrollable twitching
- Swelling in the face, lips, or tongue
- Turning blue or gray
Why You Can’t Rely on “They Look Fine”
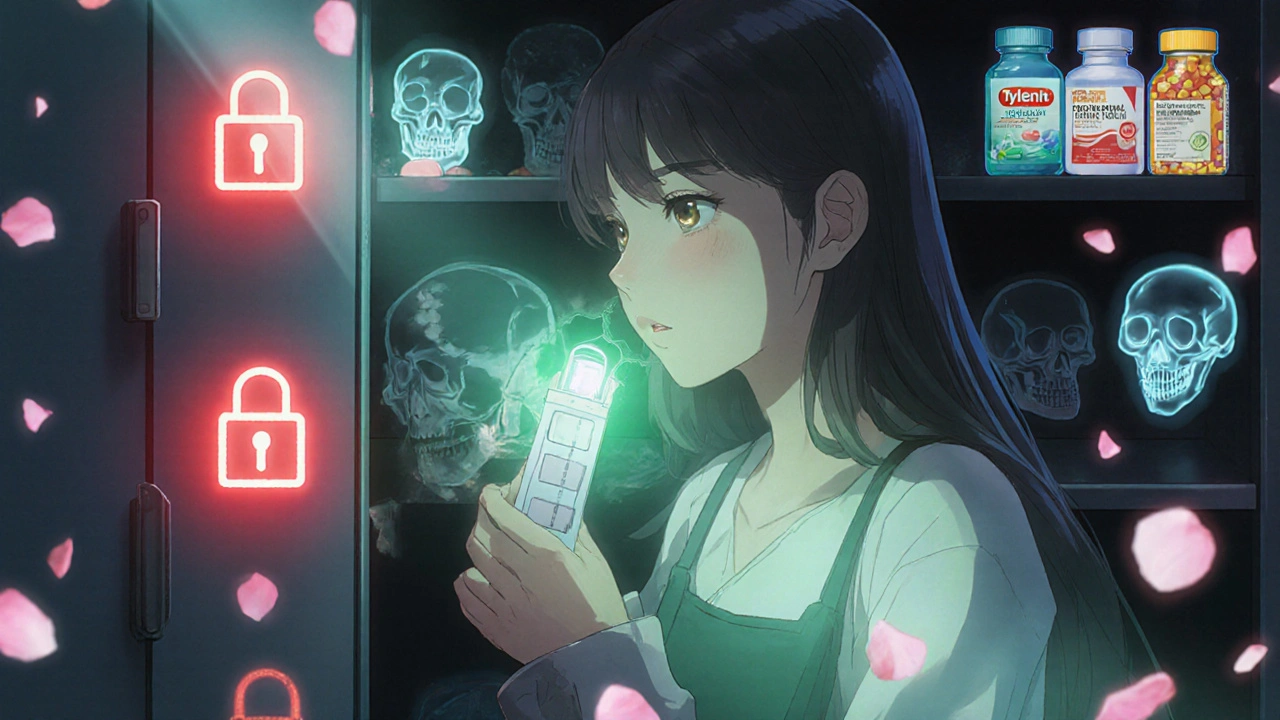
Many parents say, “But they’re smiling. They’re playing. They’re fine.” That’s the trap. Acetaminophen, opioids, and even some antidepressants can cause silent damage. The body doesn’t always scream. Sometimes it just shuts down. A 2023 study from the American Academy of Pediatrics found that 47% of all pediatric medication exposures happen in the child’s own home. In half of those cases, the medicine was left within reach - on a counter, in a purse, or in a drawer that wasn’t locked. And here’s something most parents don’t realize: Child-resistant caps aren’t enough. About 20% of poisonings happen even when bottles have those caps. Kids are smarter than we think. They twist, they chew, they use keys or scissors. Locking cabinets are the only real safety net.Prevention: What Actually Works
You can’t be perfect. But you can be smarter.- Lock it up. All meds - prescription, OTC, vitamins - go in a locked cabinet. Not a high shelf. Not a drawer. A locked cabinet. 60% of poisonings happen because the child found the meds at home.
- Never call medicine “candy.” Even jokingly. Kids hear that. They remember it.
- Read labels twice. 70% of acetaminophen overdoses happen because parents give two products with the same ingredient. Always check the active ingredient. If it says “acetaminophen” or “APAP,” don’t give another one.
- Use the right measuring tool. The FDA says 1 in 4 dosing errors happen because parents use kitchen spoons. Use the dropper, cup, or syringe that came with the medicine. Not a teaspoon.
- Check for fentanyl. If you suspect someone gave your child pills they didn’t get from a pharmacy - use a fentanyl test strip. They’re cheap, easy to use, and can save a life.
What Happens After You Call?
Poison Control will ask you:- What the child took
- How much
- When
- How old and how much they weigh
- Watch at home (with instructions)
- Go to the ER
- Go to the ER immediately
What’s Changing - and What You Need to Know
In 2020, the FDA started requiring liquid acetaminophen to be sold in single-dose packaging. Since then, accidental overdoses in kids have dropped by 19%. That’s 1 in 5 lives saved. By 2025, the FDA plans to require all liquid medications to have standardized labels and measuring devices. That means no more “5 mL” and “16 mg/mL” confusion. It’s a big step. But here’s the rising threat: medical marijuana. In 2022, there were 4,500 pediatric exposures to cannabis products - up 1,475% since 2017. Gummies, oils, and edibles look like snacks. Kids eat them. And they don’t know how strong they are. The message is clear: Everything that looks like food or candy could be poison if it’s not meant for kids.What should I do if my child swallowed a pill I didn’t see?
Call Poison Control at 800-222-1222 right away - even if you don’t know what they took. Have the pill bottle handy if possible. Don’t try to make them vomit. Don’t wait for symptoms. Poison Control will tell you whether it’s an emergency or if you can monitor at home.
Can I wait to see if my child gets sick before calling?
No. For many drugs - especially acetaminophen and opioids - damage happens before symptoms appear. Waiting could mean missing the window to save their liver or stop a fatal overdose. Call Poison Control the moment you suspect anything.
Is it safe to give my child naloxone if I think it’s an opioid overdose?
Yes. Naloxone (Narcan) is safe and won’t harm a child if opioids aren’t involved. If your child is unresponsive, breathing slowly, or has pinpoint pupils, give one dose of naloxone immediately, then call 911. You can give more doses every 2-3 minutes if they don’t wake up. It’s not risky - it’s lifesaving.
What if my child only took one extra pill?
One extra pill can be dangerous. A child’s body is small. A dose safe for an adult can be toxic for a toddler. For example, one adult Tylenol tablet (500 mg) can cause liver damage in a child under 2. Always call Poison Control - even for one pill.
Are child-resistant caps enough to keep kids safe?
No. About 20% of poisonings happen even with child-resistant caps. Kids find ways to open them - with keys, scissors, or just by twisting hard enough. The only reliable protection is a locked cabinet or high, out-of-reach lockbox.



15 Comments
mike tallent November 16, 2025 AT 21:36
Just saved this post to my phone’s home screen. 🚨 If you have kids, this isn’t optional reading - it’s survival gear. Locked cabinets. No more ‘medicine candy’ jokes. Always check APAP on labels. And yes - call Poison Control even if they’re giggling. I did. Turned out it was just a stray melatonin gummy. But what if it wasn’t? Better safe than sorry. 💪
Peter Stephen .O November 17, 2025 AT 17:07
Bro. I used to think my kid was safe because I kept meds on the top shelf. Then my 3yo opened my pill organizer with a butter knife. 🤯 Child-resistant caps? More like child-resistant-in-name-only. Now everything’s in a lockbox bolted to the floor. Also - fentanyl strips? I keep them next to the fire extinguisher. Cheap as hell. Could save a life. Seriously. Do it.
vinod mali November 18, 2025 AT 21:03
My sister in India gave her toddler a cough syrup meant for adults. No symptoms for 12 hours. Then liver failure. They barely made it. Call poison control. Always. No excuses.
Julie Roe November 20, 2025 AT 13:28
Let me tell you about the time my neighbor’s 4-year-old got into her dad’s Adderall. She was running around like a maniac, screaming at the wall, pupils blown wide. The mom thought it was ‘just energy.’ Took her 45 minutes to call. By then, the kid’s heart rate was 190. They had to intubate. This isn’t drama. It’s real. Lock it up. Read the labels. Don’t wait for ‘signs.’ The signs come too late. You’re not being paranoid - you’re being responsible.
Eva Vega November 21, 2025 AT 20:58
From a clinical toxicology perspective, the pharmacokinetic vulnerability of pediatric populations is exacerbated by developmental differences in hepatic metabolism and body weight normalization. Acetaminophen toxicity follows a dose-dependent glutathione depletion cascade, rendering NAC efficacy time-critical. The 8-hour therapeutic window is not arbitrary - it reflects hepatic cytochrome P450 saturation kinetics. Delayed presentation beyond 16 hours correlates with a 60% mortality increase due to centrilobular necrosis. Furthermore, the FDA’s standardized labeling initiative (2025) will mitigate dosing errors arising from concentration ambiguity - a documented contributor to iatrogenic injury. Vigilance is not merely prudent; it is a biomechanical imperative.
Joyce Genon November 22, 2025 AT 21:00
Ugh. Another fear-mongering post. Kids have been getting into medicine since the 1950s. We survived. Now we’re treating every accidental ingestion like a terrorist attack. Did you know 98% of pediatric exposures result in zero serious outcomes? And ‘lock everything in a cabinet’? That’s just classist nonsense. Not everyone has the space or money for a lockbox. And why are we blaming parents instead of pharmaceutical companies for making pills look like Skittles? This feels less like safety and more like control.
John Wayne November 23, 2025 AT 03:33
Interesting how the article assumes all parents are negligent. What about the ones who store meds properly but still get hit by a neighbor’s child who climbs through a window? Or the fact that some kids are just… unnaturally clever? This reads like a PSA designed to make you feel guilty, not informed. Also - fentanyl test strips? Are we now treating every child’s cough syrup like a narco-drama?
Jennie Zhu November 23, 2025 AT 04:51
While the article provides a comprehensive overview of pediatric medication exposure protocols, it neglects to address the systemic underfunding of poison control centers. In 2023, over 40% of U.S. poison control centers operated below capacity due to federal funding shortfalls. The 800-222-1222 hotline remains underutilized not due to parental ignorance, but due to inconsistent regional response times and lack of integration with EMS systems. Furthermore, the recommendation to use naloxone without confirmation of opioid ingestion may inadvertently delay definitive care in non-opioid cases. A more nuanced approach to triage is warranted.
Rob Goldstein November 24, 2025 AT 10:35
As a pediatric ER nurse, I’ve seen this a hundred times. The worst cases? The ones where parents waited because ‘they looked fine.’ One kid took one extra Tylenol. 18 hours later - liver transplant. Another took a single fentanyl patch from his grandma’s pain patch. Dead by morning. I’m not exaggerating. Lock it up. Don’t call it candy. Use the syringe. Call Poison Control. Even if you’re 1% sure. We’ve got your back. And yes - naloxone is safe. If you’re scared to use it, just remember: it’s better to give it and be wrong than to wait and regret it.
Kathy Grant November 26, 2025 AT 05:56
It’s not just about pills. It’s about the quiet, invisible fear that haunts every parent who’s ever left a bottle on the counter for five seconds. That moment when your heart drops - ‘Did I lock it?’ ‘Did I count?’ ‘Was that just a gummy or something else?’ We carry that guilt like a second heartbeat. This post doesn’t scare me - it comforts me. Because it says: you’re not alone. You’re not failing. You’re just human. And calling Poison Control? That’s not weakness. That’s love in action. I’m printing this out and taping it to my fridge.
Andrew Cairney November 27, 2025 AT 21:51
Let’s be real - this is all part of the Big Pharma / FDA mind control agenda. Why do you think they’re pushing ‘standardized labels’? To make it harder for parents to find cheaper generics. And fentanyl test strips? They’re not for kids - they’re for tracking your meds. Who’s really behind this? The same people who want you to believe ‘child-resistant caps’ are useless. Meanwhile, 90% of overdoses happen in households where the meds were prescribed - meaning the system is rigged. Don’t trust the ‘experts.’ Trust your gut. And maybe stop buying pills from pharmacies altogether.
Matt Wells November 28, 2025 AT 02:05
While the intent of the article is laudable, the prose exhibits a troubling conflation of anecdotal evidence with clinical data. The assertion that ‘one pill can kill’ is statistically misleading; the LD50 for acetaminophen in a 10kg child is approximately 150mg/kg, meaning a single 500mg tablet would require a body weight of less than 3.3kg to be lethal - an implausible scenario. Furthermore, the recommendation to administer naloxone in non-confirmed opioid cases lacks rigorous pharmacological justification. The article, while emotionally compelling, fails to meet the standards of evidence-based public health communication.
Gary Lam November 29, 2025 AT 11:33
Y’all in the U.S. are wild. In my country, we just leave meds on the counter and let the kids figure it out. My cousin’s kid ate three Advil and then asked for a snack. No big deal. You know what saved him? A glass of milk and a nap. Maybe stop treating every child like a lab rat. Also - why is everyone so scared of Tylenol? It’s not cocaine. 😅
Jennifer Howard November 29, 2025 AT 23:22
It’s not just the meds - it’s the culture of irresponsibility. Parents who don’t read labels, who don’t lock things up, who call it ‘candy’ and then wonder why their child is in the ER. And don’t get me started on the ‘poison control’ obsession - it’s a crutch for lazy parenting. If you can’t be bothered to know what’s in your medicine cabinet, then maybe you shouldn’t have children. I’ve raised two kids without a single lockbox. We used common sense. And guess what? They’re healthy. This article is a symptom of a society that’s lost its moral compass.
Abdul Mubeen December 1, 2025 AT 00:56
Are we sure these ‘pediatric overdoses’ aren’t being inflated to justify increased surveillance? Who benefits from parents being terrified of their own medicine cabinets? The pharmaceutical industry? The government? The ‘Poison Control’ system? The fact that this article doesn’t question the source of the 1 million exposure statistic is suspicious. And why are we not talking about the fact that many of these cases involve unregulated online pharmacies? This feels less like public health and more like social engineering.