When you’re living with an autoimmune disease like rheumatoid arthritis, multiple sclerosis, or lupus, every treatment choice feels like a gamble. One drug might slash your flare-ups by 60%, but it could also raise your risk of a rare but deadly brain infection. Another might be safer but leave you with constant fatigue that makes it hard to work or care for your kids. In these situations, no doctor can decide for you - not because they don’t care, but because shared decision-making is the only way to get it right.
What Shared Decision-Making Really Means
Shared decision-making isn’t just asking, “What do you want to do?” It’s a structured process where you and your provider sit down with clear data, talk through what matters most to you, and pick a path together. This isn’t new. The idea started gaining ground in the 1980s, but it only became standard care for chronic conditions like autoimmune diseases after 2010. Today, groups like the American College of Rheumatology and the American Academy of Neurology say it’s not optional - it’s required.Here’s how it works: Your doctor doesn’t just hand you a list of drugs. They show you real numbers. Not vague terms like “low risk” or “high chance.” Actual stats: “For every 1,000 people on this medication, 1 might get PML - a brain infection that can be fatal.” Or, “Out of 100 people like you, 60 will see major improvement with this drug, but 20 will get a serious infection within a year.”
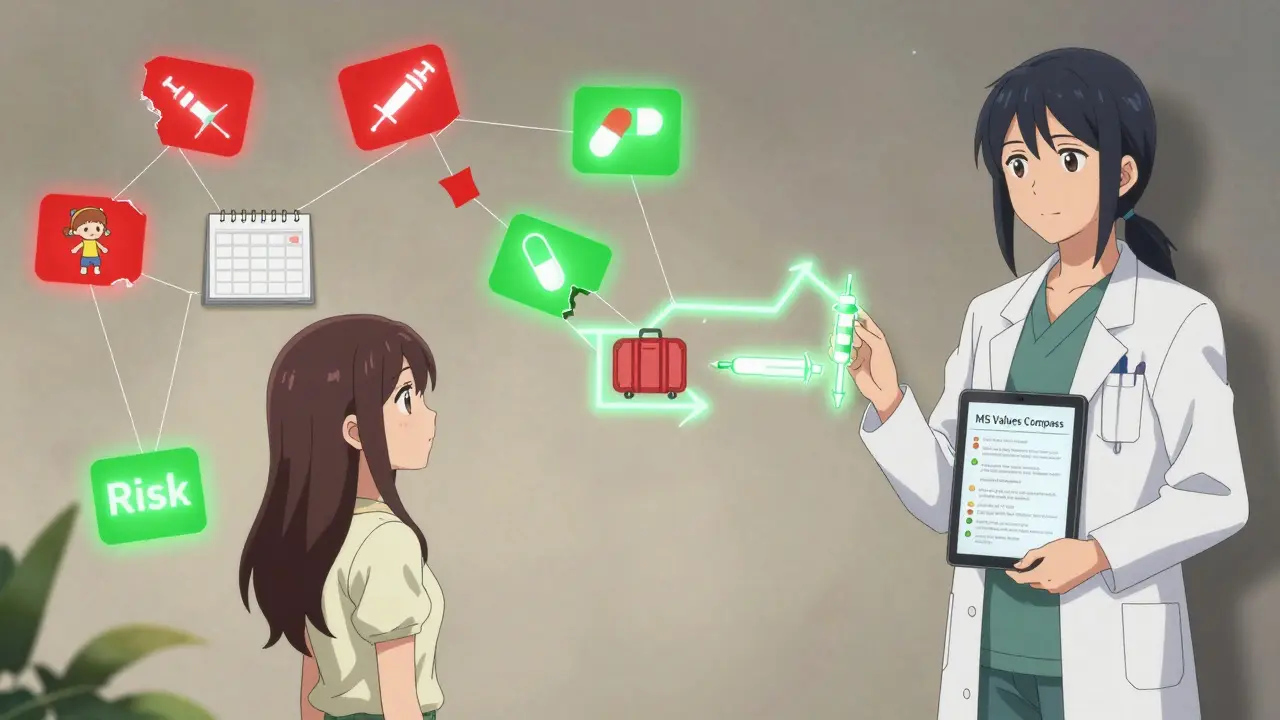
These numbers come from decision aids - free tools made by hospitals and patient groups. The Arthritis Foundation has them for RA, psoriatic arthritis, and lupus. The National MS Society offers one called “MS Values” that helps you rank what matters most: Can you live with weekly injections? Are you okay with monthly infusions? Is traveling often a dealbreaker? These tools turn abstract fears into concrete choices.
Why This Beats the Old Way
For decades, doctors made the calls. That’s the paternalistic model. Or, sometimes, they just gave you a list and said, “Pick one.” That’s the informative model. Neither works well for autoimmune diseases.A 2017 study of over 3,200 patients with autoimmune conditions found that those who took part in shared decision-making stuck with their treatment 82% of the time. Those who didn’t? Only 63%. That’s not a small gap. That’s a 30% drop in adherence - meaning more flares, more hospital visits, more cost.
And the cost isn’t just financial. Inflammatory bowel disease patients who used shared decision-making spent $18,452 a year on care. Those who didn’t? $22,231. That’s nearly $4,000 less per person - because they weren’t cycling through ineffective treatments or ending up in the ER.
Shared decision-making works best when there’s no single “best” option. For example: If you’re a nurse who works night shifts, a daily pill might be better than a weekly injection you can’t remember to take. If you’re planning a pregnancy, some biologics are safe - others aren’t. If you’re terrified of needles, an oral drug might be worth a slightly higher risk of side effects. Your values matter. Your life matters. That’s why this process exists.
What Goes Wrong
It sounds simple. But in practice, it often doesn’t happen.A 2021 survey of rheumatologists found that 78% said they don’t have enough time. A 15-minute appointment? That’s not enough to explain PML risk, ask about your job, your family, your fears - and still make a plan.
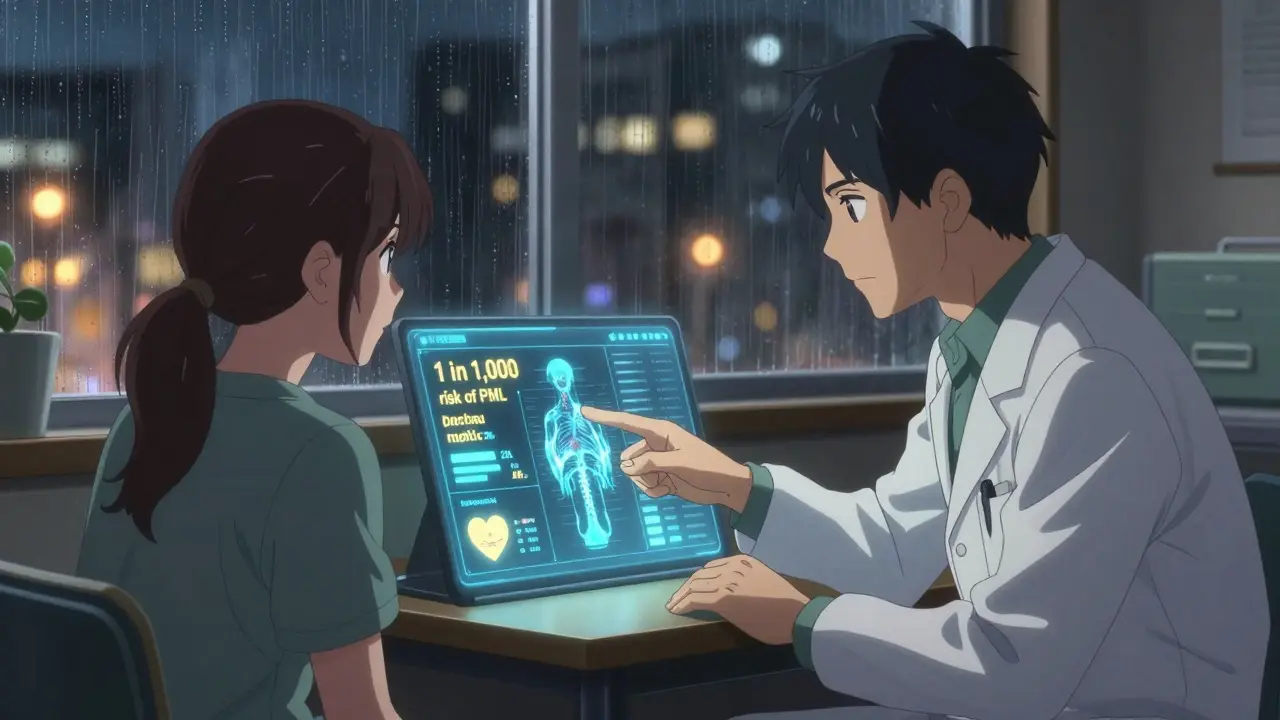
And then there’s the way risk is presented. One patient told me: “My neurologist said, ‘There’s a 0.1% chance of PML.’ I didn’t even know what that meant. Then he showed me a chart: ‘1 in 1,000.’ That’s when it hit me. That’s like one person in a full stadium. Suddenly, it felt real.”
That’s the difference between relative and absolute risk. Saying “your risk is reduced by 50%” sounds scary. Saying “your risk goes from 2 in 1,000 to 1 in 1,000” is clearer. Good providers use absolute numbers. Bad ones hide behind percentages.
Another problem? Patients feel rushed. A 2020 survey by the National MS Society found 63% of patients felt like their doctors didn’t listen. One woman said: “He listed three drugs in 90 seconds. Didn’t ask if I had kids. Didn’t ask if I could afford the copay. Just said, ‘Which one do you want?’”
When this happens, people stop taking their meds. A 2019 study found 38% of biologic therapy stoppages weren’t because the drugs didn’t work - they were because the treatment didn’t fit the patient’s life.
How to Make It Work for You
You don’t have to wait for your doctor to bring it up. You can start it.Before your appointment, go to Arthritis Foundation or National MS Society and download their decision aids. Fill them out. Write down what matters most: your job, your energy levels, your fear of side effects, your budget.
At the visit, say this: “I’ve been thinking about my options. Can we go through the risks and benefits together? I want to make sure this fits my life.”
Ask for numbers. Not “some risk,” but “how many out of 100?” Ask: “What happens if I wait six months?” “What if I try the pill first?” “What’s the worst thing that could happen?”
Bring someone with you. A spouse, a friend, a caregiver. Two ears are better than one. You’ll forget half of what’s said.
And if your provider dismisses you? Get a second opinion. You have the right to be heard.

What’s New in 2026
Technology is helping. In March 2023, the FDA cleared the first AI-powered tool for rheumatoid arthritis called ArthritisIQ. It pulls data from your EHR, your symptom logs, even your sleep patterns, and generates a personalized risk-benefit report. It doesn’t decide for you - it just makes the data clearer.The MS Association launched “MS Values Compass” in early 2023. It’s a digital tool that asks you to rank 10 treatment traits - like “I want to avoid infusions,” or “I need to travel often.” It then matches you to drugs that fit your profile. Over 12,000 people have used it in six months.
Insurance is catching up too. Medicare now ties 9% of payments to patient satisfaction scores - and shared decision-making is a big part of that. European guidelines now require documentation of shared decisions before starting biologics. In the U.S., that’s still rare - only 32% of providers document it properly.
But here’s the catch: Digital tools help younger, tech-savvy patients. A 2022 study found patients over 65 and those with lower health literacy get 37% less benefit from apps and websites - unless they get in-person help. That’s why the best systems combine tech with human support.
What This Means for Your Future
Autoimmune diseases aren’t curable. But they’re manageable - if you’re in the driver’s seat.Shared decision-making isn’t about being “difficult.” It’s about being informed. It’s about knowing that your life - your schedule, your fears, your dreams - matters just as much as the lab results.
The data doesn’t lie: When patients are truly involved, they stick with treatment longer. They spend less on care. They feel more in control. And they’re less likely to regret their choices.
This isn’t about picking the “best” drug. It’s about picking the right one - for you.
What’s the difference between shared decision-making and just getting a second opinion?
A second opinion gives you another doctor’s take. Shared decision-making is a process where you and your current provider work together using evidence and your personal values to choose a path. You don’t need a new doctor - you need better communication with the one you have.
Can I use shared decision-making during a flare-up?
Not always. During severe flares - like a sudden MS relapse or a lupus kidney crisis - you need fast action. There’s no time for a 10-minute discussion. But once the crisis is under control, that’s when shared decision-making kicks in: choosing what comes next, not just what’s needed now.
Are decision aids only for biologics?
No. They’re used for any treatment with meaningful trade-offs: oral DMARDs vs. biologics, steroid tapering plans, switching from injectables to pills, even choosing between different MS therapies. If there’s more than one reasonable option - and each has different risks - you need a decision aid.
What if my doctor says they don’t have time?
Say this: “I understand time is tight. Can we schedule a 15-minute follow-up just to go over my options with the decision aid? I’ve already filled it out.” Many providers will agree - especially if you show you’re prepared. Pre-visit tools cut discussion time by over 3 minutes.
Do I have to pay for decision aids?
No. The Arthritis Foundation, National MS Society, and major hospitals offer them for free. Some are apps, some are booklets, some are videos. You can download them on your phone before your appointment. There’s no cost, no subscription, no catch.
How do I know if my doctor is good at shared decision-making?
Look for these signs: They ask what matters most to you. They show you numbers in absolute terms (like “1 in 100”) not percentages. They pause and let you respond. They don’t push one option. They say, “There’s no right answer - only the right one for you.” If they talk more than you, they’re not doing it right.


9 Comments
Pooja Kumari January 9, 2026 AT 08:31
I’ve been on biologics for 7 years and let me tell you, this post hit me right in the feels. I remember sitting in that office, my hands shaking, the doctor saying ‘it’s a 0.1% chance’ like it was a rain forecast. I went home and cried for an hour because I thought I was being dramatic. Then I found that MS Values tool and it changed everything. Suddenly, I wasn’t just a patient number-I was someone who needed to hold her kids without collapsing. I chose the oral med. I get tired. I miss work sometimes. But I’m alive. And I got to watch my daughter’s first ballet recital. No drug is worth missing that. I wish every doctor had to sit through one of my flare-ups before they could prescribe anything.
Jacob Paterson January 10, 2026 AT 01:57
Oh please. You all act like you’re fighting for your life when you just don’t want to take your meds. ‘I’m scared of needles’? Get over it. I’ve been on 12 different immunosuppressants and I didn’t cry once. You people treat your autoimmune disease like it’s a Netflix show you can pause when it gets uncomfortable. The stats don’t care about your ‘values.’ They care about survival. If you can’t handle a 0.1% risk, maybe you shouldn’t be out in public. You’re not special. You’re just lazy.
Angela Stanton January 10, 2026 AT 22:46
Let’s contextualize this within the risk-benefit matrix of modern immunomodulatory therapeutics. The 2017 adherence data (82% vs 63%) is statistically significant (p<0.001), but the effect size is confounded by selection bias-patients who engage in shared decision-making are inherently more health-literate and socioeconomically advantaged. Also, the ‘$4,000 savings’ metric ignores indirect costs like lost productivity and caregiver burden. And let’s not forget the placebo effect in patient-reported outcomes. The real issue? Systemic underfunding of rheumatology clinics. AI tools like ArthritisIQ are band-aids on a hemorrhaging system. We need structural reform, not patient empowerment theater.
Johanna Baxter January 11, 2026 AT 18:43
My doc said ‘1 in 1000’ and I thought it meant I’d be fine… then I saw a woman in the waiting room with a feeding tube and I lost it. I cried in the parking lot. I didn’t even know what PML was until I googled it at 2am. I took the pill. I’m tired all the time. My husband says I’m not the same. I don’t care. I’m alive. And I don’t wanna die because someone thought I was ‘too emotional’ to make a choice. I’m not a statistic. I’m a mom. And I’m done being polite about this.
Jerian Lewis January 11, 2026 AT 23:23
I appreciate the intent behind shared decision-making, but it’s a luxury. Most people don’t have the mental bandwidth to parse risk ratios after a 12-hour shift, managing kids, and paying bills. The system is designed to make patients feel responsible for outcomes they can’t control. The real problem isn’t that patients aren’t involved-it’s that the system doesn’t give them the time, energy, or resources to participate meaningfully. This isn’t empowerment. It’s burden-shifting.
Kiruthiga Udayakumar January 12, 2026 AT 11:02
As someone from India who traveled 600km for a rheumatologist, I can tell you-no one here even knows what shared decision-making is. My doctor handed me a script and said ‘take this or you’ll be in a wheelchair.’ I found the Arthritis Foundation website on my phone in the hospital lobby. I printed the decision aid. I showed it to him. He rolled his eyes and said ‘you’re too educated for your own good.’ I’m still on the pill. I’m still here. And I’m not apologizing for asking questions. You don’t get to decide what my life is worth.
Patty Walters January 12, 2026 AT 17:43
Just a quick thing-when you ask for numbers, ask for absolute risk, not relative. Like, if they say ‘50% lower risk,’ ask ‘so from what to what?’ I used to get scared by ‘reduced risk’ until someone explained it: ‘from 2 in 1000 to 1 in 1000’-that’s like flipping a coin once a year and hoping it doesn’t land on heads. Also, bring a notebook. Or a voice recorder. You’ll forget half of it. And it’s okay to say ‘I need to think about this.’ No one’s gonna judge you. Really.
Phil Kemling January 14, 2026 AT 02:59
Shared decision-making is just a fancy term for acknowledging that medicine isn’t a science-it’s a conversation between two humans, one of whom is terrified and the other of whom is exhausted. The data gives us options, but not answers. The answer is always in the silence between the words. In the way someone hesitates before saying ‘I’m scared.’ In the way they look at their hands when they talk about their kid. That’s where the real diagnosis happens. The numbers just help us name what we already feel.
tali murah January 14, 2026 AT 14:55
How is it that in 2026, we’re still treating patients like children who need to be ‘guided’ through decisions that could kill them? The real tragedy isn’t that doctors don’t have time-it’s that they still think their opinion matters more than the patient’s lived experience. You don’t get to decide what ‘quality of life’ means for someone else. And if your ‘risk’ is someone else’s daily reality? Then your risk is a privilege. This isn’t medicine. It’s moral theater. And I’m done watching.