When your urine looks foamy, especially after you’ve been standing for a while, it’s easy to brush it off as just water turbulence. But if that foam sticks around, it could be your body’s quiet signal that something’s wrong with your kidneys. Proteinuria - excess protein in your urine - isn’t a disease on its own. It’s a warning sign. And left unchecked, it can lead to permanent kidney damage.
What Exactly Is Proteinuria?
Your kidneys are like high-precision filters. They let waste and extra water out through urine, but they’re designed to keep proteins like albumin inside your bloodstream. Albumin helps maintain fluid balance, carries hormones, and supports tissue repair. When these filters get damaged - from high blood pressure, diabetes, or inflammation - proteins leak out. That’s proteinuria.
Healthy kidneys let through less than 150 milligrams of protein per day. Anything above that is abnormal. But here’s the catch: you won’t always feel it. In fact, 70% of people with early-stage proteinuria have no symptoms at all. That’s why testing matters more than waiting for signs.
How Is It Detected?
Detecting proteinuria starts simple: a urine dipstick test. Your doctor puts a chemically treated strip in your sample, and it changes color if protein is present. It’s fast, cheap, and widely used. But it’s not perfect. Dipsticks can miss low levels of protein or give false positives if you’re dehydrated or have a urinary infection.
For accuracy, doctors rely on two tests:
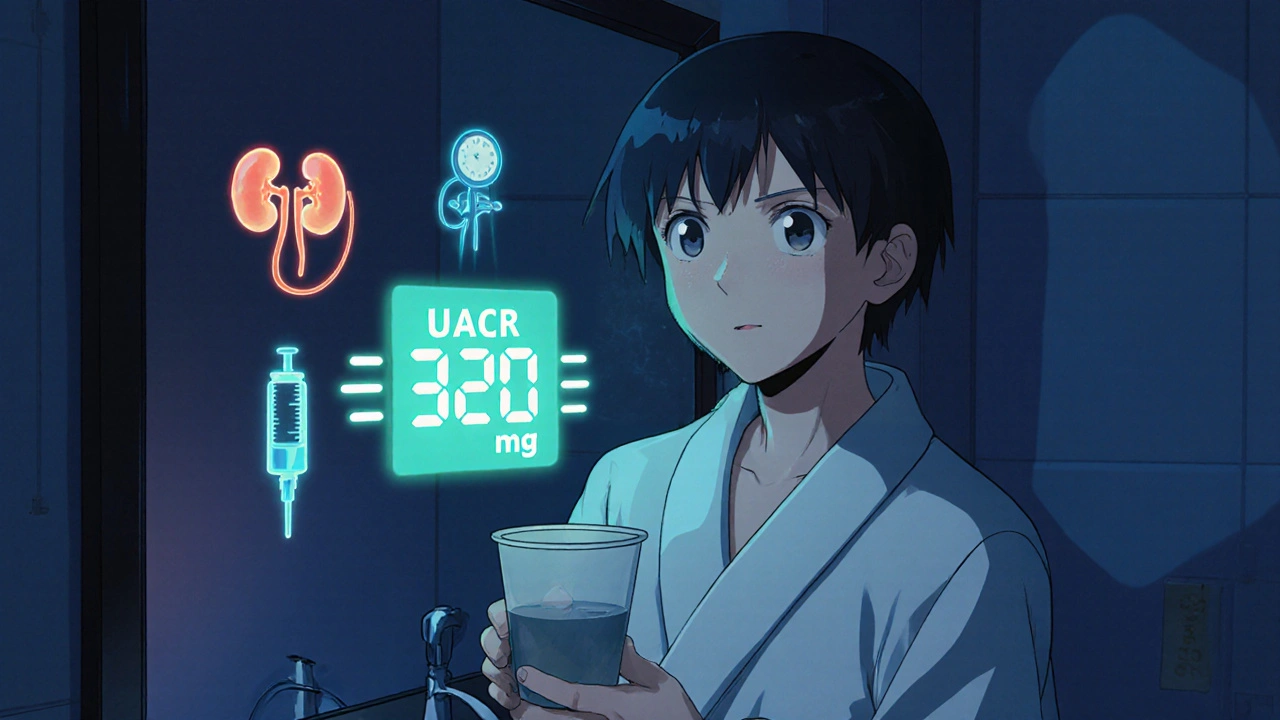
- Urine albumin-to-creatinine ratio (UACR): A single urine sample, measured in milligrams of albumin per gram of creatinine. A value over 30 mg/g is considered abnormal. This is now the gold standard for screening.
- 24-hour urine collection: You collect all your urine over a full day. It’s more precise but harder to do correctly. Many people forget a sample or spill some, which throws off results.
For people with diabetes or high blood pressure, annual UACR testing is standard. If your UACR is between 30 and 300 mg/g, you have moderate proteinuria. Above 300 mg/g? That’s severe - and it means your kidneys are under serious stress.
Why Does It Happen?
Not all proteinuria is the same. There are three main types:
- Transient: Comes and goes. Triggered by fever, intense exercise, dehydration, or extreme stress. It’s harmless and resolves on its own.
- Orthostatic: Happens only when you’re upright. Common in teens and young adults. Protein disappears in morning urine after lying down all night. Usually not a problem.
- Persistent: Always there. This is the red flag. It’s linked to underlying disease.
Most persistent cases come from just a few causes:
- Diabetes: Accounts for 40% of cases. High blood sugar damages the kidney’s filtering units over time.
- High blood pressure: Responsible for 25%. Constant pressure on kidney vessels leads to leaks.
- Glomerulonephritis: Inflammation of the kidney’s filtering clusters. Makes up 15% of cases.
- Lupus and other autoimmune diseases: Your immune system attacks your kidneys. Seen in about 7% of cases.
- Preeclampsia: A pregnancy complication that causes sudden proteinuria and high blood pressure.
Less common causes include multiple myeloma, amyloidosis, and severe heart failure. But if you’re diabetic or hypertensive, those are your biggest risks.
What Are the Symptoms?
Early proteinuria? Often silent. But as protein loss grows, your body starts to show signs:
- Foamy or bubbly urine: The most common visible sign. Caused by protein disrupting surface tension.
- Swelling (edema): Especially in ankles, feet, hands, and around the eyes. Your body loses albumin, so fluid leaks into tissues.
- Fatigue and weakness: Your body can’t repair tissues properly without enough protein.
- Weight gain: From fluid retention, not fat.
- Nausea or loss of appetite: When kidney function drops, waste builds up in your blood.
If you’re losing more than 3,500 mg of protein daily, you may develop nephrotic syndrome: severe swelling, low blood albumin, high cholesterol, and increased clotting risk. This needs urgent care.
How Do You Stop It From Worsening?
Proteinuria isn’t just a symptom - it’s a driver of damage. The more protein you lose, the faster your kidneys decline. Studies show that people excreting over 1 gram of protein per day have a 50% chance of reaching kidney failure within 10 years - unless they act.
Here’s what actually works:
1. Control Your Blood Pressure
Keep it under 130/80 mmHg. Every 10-point drop in systolic pressure reduces proteinuria by about 15%. ACE inhibitors (like lisinopril) and ARBs (like losartan) are first-line drugs. They don’t just lower blood pressure - they directly protect the kidney filters. In fact, they reduce protein loss by 30-50%.
Side note: Some people stop taking them because of a dry cough. Talk to your doctor. There are alternatives.
2. Manage Blood Sugar (If You Have Diabetes)
Keeping HbA1c below 7% slows kidney damage. But newer drugs like SGLT2 inhibitors (canagliflozin, dapagliflozin) go further. They reduce proteinuria by 30-40% and cut the risk of kidney failure by 30%. These are now recommended for all diabetics with proteinuria, even if their blood sugar is under control.
3. Diet Matters - But Don’t Go Too Low
Many think cutting protein will help. It does - but only up to a point. A moderate protein intake of 0.6-0.8 grams per kilogram of body weight per day reduces kidney strain. For a 70 kg person, that’s 42-56 grams daily. Too little, and you risk muscle loss and malnutrition.
Focus on high-quality protein: eggs, fish, lean poultry, tofu. Avoid processed meats and excess salt. Salt makes swelling worse and raises blood pressure.
4. Medications Beyond ACE/ARBs
For autoimmune causes like lupus nephritis, steroids and rituximab can bring proteinuria into remission in 60-70% of cases.
Newer drugs like finerenone (a non-steroidal mineralocorticoid blocker) reduce proteinuria by 32% in diabetic kidney disease and slow decline in kidney function. It’s now approved in the U.S. and Europe for this use.
How Often Should You Get Tested?
Screening isn’t for everyone. But if you have risk factors, don’t skip it:
- Diabetics: Test UACR every year. If you’re on treatment, check every 3-6 months.
- Hypertensives: Same as diabetics - annual testing.
- Family history of kidney disease: Start testing at age 40.
- Obese or sedentary: If you have other metabolic issues, get screened every 2 years.
For people with confirmed proteinuria, monitoring frequency depends on severity:
- UACR 30-300 mg/g: Every 6 months
- UACR >300 mg/g: Every 3 months
- During treatment: Monthly until levels drop by 30% or more
Tracking your progress matters. A 30% reduction in proteinuria within 3 months means your treatment is working - and your kidneys are being protected.
What’s New in Testing and Treatment?
Technology is catching up. Smartphone apps that analyze urine color and foam with a camera are now 85% accurate compared to lab tests. They’re not replacements, but they’re great for tracking changes at home.
Researchers are also finding new biomarkers. One study identified elevated urinary TNF receptor-1 as a predictor of rapid kidney decline - even before proteinuria gets worse. That could lead to earlier, more targeted treatment.
For rare genetic conditions like Alport syndrome, a drug called bardoxolone methyl is showing promise in trials, cutting proteinuria by 35%. These are still experimental, but they point to a future where treatment is personalized based on your genetics and biomarkers.
What Should You Do Right Now?
If you’re worried about proteinuria:
- Ask your doctor for a UACR test - especially if you’re diabetic, hypertensive, or have a family history.
- If your result is abnormal, don’t panic. Repeat it. One high reading isn’t a diagnosis.
- If confirmed, get evaluated for underlying causes within two weeks.
- Start lifestyle changes: reduce salt, control blood pressure and sugar, eat moderate protein.
- Follow up with your doctor every 3-6 months. Track your numbers.
Proteinuria is not a death sentence. It’s a measurable warning. And the earlier you act, the more you can protect your kidneys. Many people with proteinuria live normal, healthy lives - as long as they pay attention to the signs and stick with their treatment.
Can You Reverse It?
Yes - sometimes. In early stages, especially with diabetes or high blood pressure, reducing proteinuria can actually reverse some kidney damage. Studies show that patients who cut their protein loss by 50% lower their risk of kidney failure by 30%. The key is consistency: medication, diet, and monitoring. No shortcuts.
But if proteinuria has been high for years, the damage may be permanent. That’s why early detection is everything.
Is foamy urine always a sign of kidney problems?
Not always. Foamy urine can happen after vigorous urination, dehydration, or even from toilet cleaning products. But if the foam is fine, persistent, and doesn’t go away after a few minutes - especially if you also have swelling or fatigue - it’s worth getting checked. A simple UACR test can rule out proteinuria.
Can I test for proteinuria at home?
Yes, but with limits. Over-the-counter dipstick tests are available and can detect moderate to high levels of protein. But they can’t measure exact amounts or detect early-stage proteinuria. For accurate results, a lab-based UACR test is still the gold standard. Home tests are best for tracking known conditions, not for initial diagnosis.
Does drinking more water reduce protein in urine?
No. Drinking more water dilutes your urine, which might make foam less obvious - but it doesn’t reduce the actual amount of protein your kidneys are leaking. Treating the root cause - like high blood pressure or diabetes - is the only way to lower proteinuria long-term.
Can proteinuria go away on its own?
Yes - but only if it’s transient. If it’s caused by fever, exercise, or stress, it usually resolves once the trigger is gone. Persistent proteinuria, however, won’t disappear without treating the underlying condition. Ignoring it risks permanent kidney damage.
Are there foods that worsen proteinuria?
Yes. High-sodium foods (processed snacks, canned soups, fast food) increase swelling and blood pressure, making proteinuria worse. Excess animal protein (red meat, full-fat dairy) can also strain kidneys if you already have damage. Stick to plant-based proteins, fish, and lean poultry in moderate amounts.
Should I avoid protein supplements if I have proteinuria?
Yes. Protein powders, especially whey or casein, add extra protein your kidneys can’t handle. Even if you’re trying to build muscle, excess protein increases kidney workload. Talk to a renal dietitian before taking any supplements.
Can proteinuria lead to dialysis?
It can - but it doesn’t have to. People with persistent, untreated proteinuria have a much higher risk of progressing to kidney failure. However, with early detection and proper treatment - controlling blood pressure, managing diabetes, and using kidney-protective drugs - many people never reach dialysis. The goal is to reduce protein loss and slow decline.


10 Comments
Charmaine Barcelon November 23, 2025 AT 22:50
Foamy urine?? I saw that once after I drank a protein shake and thought I was dying. Turns out I was just dehydrated. But now I’m paranoid every time I pee. You people need to stop scaring everyone with this stuff.
Karla Morales November 25, 2025 AT 08:26
⚠️ IMPORTANT: Proteinuria is NOT a joke. If you're diabetic or hypertensive and ignoring foamy urine, you're playing Russian roulette with your kidneys. 🚨 UACR testing is cheap, non-invasive, and saves lives. Stop waiting for symptoms. Get tested. Now. 📊🩺
Javier Rain November 27, 2025 AT 07:31
Yo, this post is gold. I’ve been on losartan for 3 years and my UACR dropped from 420 to 85. It’s not magic-it’s discipline. Blood pressure control + SGLT2 inhibitors = game changer. If you’ve got proteinuria, don’t wait. Talk to your doc about finerenone too. It’s a newer option that actually works. You’ve got this.
Laurie Sala November 28, 2025 AT 00:51
I’ve had proteinuria for 7 years… and I cried when I first saw the numbers… I thought I was going to die… my mom had kidney failure… I’ve been on ACE inhibitors since 2018… I still get scared every time I pee… please, please, please don’t ignore this… I’m still here… but I almost wasn’t…
Lisa Detanna November 28, 2025 AT 11:34
In my culture, we don’t talk about pee much-but I’m glad this post breaks the silence. In my village in Mexico, people think kidney problems only happen to old people. But diabetes is spreading fast. We need more education. Maybe translate this into Spanish? I’ll help. This info saves lives.
Demi-Louise Brown November 29, 2025 AT 19:15
Consistency matters more than perfection. One small step: track your blood pressure daily. One small step: swap chips for almonds. One small step: schedule that UACR test. Progress isn’t loud. It’s quiet. And it’s powerful.
Matthew Mahar November 30, 2025 AT 10:29
wait so if i drink more water it dont help?? but i thought water flushes everything out?? like my kidneys are just... leaking?? like a broken hose?? this makes me feel so helpless
John Mackaill November 30, 2025 AT 17:49
Good point about the home tests. I use the dipsticks monthly to track trends, but I still get the lab UACR every 6 months. They’re useful for spotting changes between visits. Just don’t rely on them for diagnosis. I learned that the hard way.
Adrian Rios December 2, 2025 AT 09:53
I want to emphasize something the post barely touches on: proteinuria isn’t just about kidneys-it’s a systemic signal. When your kidneys leak protein, your vascular system is under stress, your inflammation markers are up, and your heart is working harder. That’s why ACE inhibitors and SGLT2 inhibitors don’t just protect the kidneys-they reduce heart attacks and strokes too. This isn’t a kidney issue. It’s a whole-body wake-up call. And if you’re on steroids for lupus nephritis? Don’t stop them just because you feel better. Remission isn’t cure. Keep monitoring. Your future self will thank you.
Casper van Hoof December 3, 2025 AT 06:32
One might posit that proteinuria, as a biomarker, represents the ontological fragility of human homeostasis-our biological systems, finely tuned over millennia, now rendered vulnerable by the very advancements of modernity: processed foods, sedentary lifestyles, and chronic stress. The body, in its quiet way, whispers its dissent through albumin in urine. To ignore this whisper is to deny the dialogue between organism and environment. The cure, then, is not merely pharmacological, but existential: a reclamation of rhythm, balance, and reverence for the body’s innate wisdom.