It’s 2025, and you’ve been taking generic metformin for type 2 diabetes for three years. Your prescription is refilled automatically. Then one day, your pharmacy says: "We can’t fill this. Your insurance needs prior authorization." You’re confused. This isn’t a $10,000 specialty drug. It’s a $4 generic pill that’s been the standard of care for decades. Why does your insurance now need to approve it?
Why Generics Need Approval Now
For years, generic drugs were the easy win in healthcare. They’re cheaper, just as effective, and rarely required extra steps. But that’s changed. In 2024, 15-20% of generic prescriptions required prior authorization-up from just 5% in 2018. That’s not a typo. Insurance companies, through their pharmacy benefit managers (PBMs), are now putting the same red tape on cheap, proven generics as they do on expensive brand-name drugs. This isn’t about saving money. It’s about control. PBMs collect $138.7 billion a year in rebates and fees. When a patient switches from one generic to another-even if both are equally effective-the PBM might earn a bigger kickback. So they make you jump through hoops to get the one they want you to use.How the Process Works
When your doctor writes a prescription for a generic drug that needs prior authorization, they have to submit paperwork to your insurer. This can be done electronically, by fax, or over the phone. The insurer then checks if your case meets their rules. These rules vary wildly:- You might need proof you tried another generic first (step therapy)
- You might need lab results showing your condition isn’t improving
- You might need a letter from your doctor explaining why this specific generic is necessary
When It Goes Wrong
Delays aren’t just annoying-they’re dangerous. A 2023 American Medical Association survey found that 24% of physicians have seen patients hospitalized because of prior authorization delays. In one documented case, a patient with diabetes waited 14 days for approval to get generic metformin. During that time, their HbA1c jumped from 6.8% to 8.2%. That’s not a small bump. That’s a spike into dangerous territory. Even common drugs like lisinopril (for high blood pressure), levothyroxine (for hypothyroidism), and atorvastatin (for cholesterol) now require prior authorization in some plans. These aren’t experimental drugs. They’re the foundation of chronic disease management.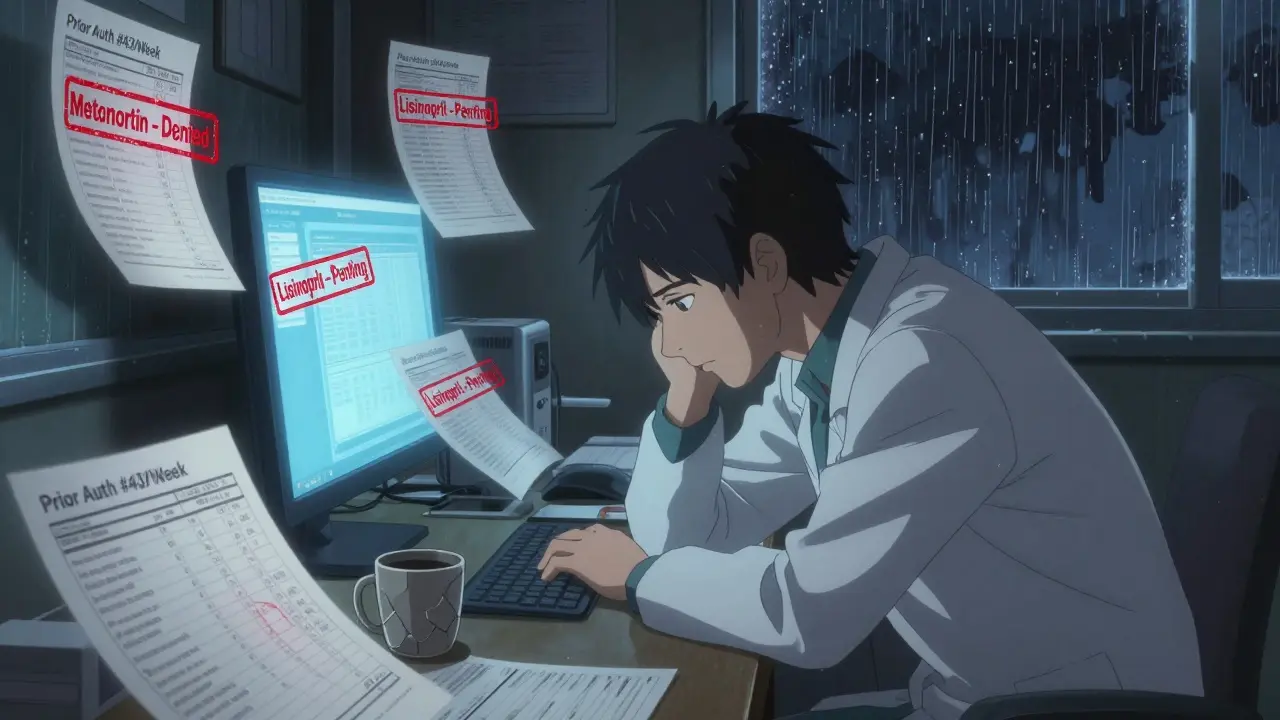
Who’s Doing It-and Why
Not all insurers treat generics the same. In 2024:- Aetna required prior authorization for 25% of its generic formulary
- UnitedHealthcare required it for 22%
- Humana required it for 18%
What’s Changing in 2025 and Beyond
There’s pushback. In January 2025, California passed SB 1024, banning prior authorization for 47 essential generic drugs on the state’s Essential Drug List. Other states are following. At the federal level, the 2024 Improving Seniors’ Timely Access to Care Act requires Medicare Advantage plans to use electronic prior authorization and respond to urgent requests within 72 hours. That’s a start. Even insurers are backing down. On June 23, 2025, six major companies-Aetna, UnitedHealthcare, Cigna, Humana, Elevance Health, and Blue Cross Blue Shield-announced they would eliminate prior authorization for 12 common generic classes by January 2026. Those include:- ACE inhibitors (like lisinopril)
- Statins (like atorvastatin)
- Metformin
- Levothyroxine
- Hydrochlorothiazide

What You Can Do
If your generic prescription gets flagged:- Ask your doctor to submit the request electronically. Studies show this cuts approval time by 32% compared to fax or phone.
- Request an "urgent" review if your condition could worsen. Cigna processes urgent requests in 72 hours-though some insurers still drag their feet.
- Keep copies of every communication. About 67% of denials can be overturned with better documentation.
- Check if your state has banned prior auth for certain generics. California, Oregon, and several others have new rules.
- Call your insurer’s member services. Ask: "Is this drug on your formulary without prior authorization?" If they say yes, but your pharmacy says no, escalate it.
What’s Next
The tide is turning. The Congressional Budget Office projects a 40% drop in prior authorization for generics by 2028-if current reforms keep moving. But until then, patients and providers are stuck in a broken system. Generics were supposed to make healthcare simpler and cheaper. Now, they’re caught in a web of bureaucracy that costs time, money, and sometimes lives. The goal shouldn’t be to approve every generic. The goal should be to stop treating them like they need approval at all.Why would insurance require prior authorization for a cheap generic drug?
Insurance companies use prior authorization to control which drugs are dispensed, even if they’re low-cost. While brand-name drugs are often blocked to push patients toward generics, some insurers now restrict generics too-usually to steer patients toward a specific generic version that gives the pharmacy benefit manager a higher rebate. It’s not about cost savings; it’s about profit control.
Which common generic drugs are most likely to need prior authorization?
In 2025, the most common generics requiring prior authorization include metformin, lisinopril, levothyroxine, atorvastatin, and hydrochlorothiazide. Even older, well-established drugs like methotrexate and sulfasalazine are now flagged in some plans, especially for autoimmune conditions. Specialty generics-like those used in cancer or inflammatory diseases-are the most likely to require approval.
How long does prior authorization for generics usually take?
Standard requests can take 5-10 business days. Some insurers, like Cigna, say 72 hours for urgent cases, but in practice, delays often stretch into weeks. Electronic submissions cut approval time by 32% compared to fax or phone. If your condition is unstable, always ask for an "urgent" review.
Can I appeal a denied prior authorization for a generic drug?
Yes. About 67% of denials are overturned on appeal with better documentation. Your doctor should submit clinical notes, lab results, and proof of previous treatment failures. Keep records of all communications. If the denial is based on a formulary rule that contradicts medical guidelines, cite those guidelines in your appeal.
Are there states that ban prior authorization for generics?
Yes. California’s SB 1024, effective January 2025, prohibits prior authorization for 47 essential generic drugs on its Essential Drug List. Other states, including Oregon and New York, have passed similar restrictions for high-use generics like metformin and levothyroxine. Check your state’s health department website for updated rules.
Will prior authorization for generics go away completely?
It’s likely. Major insurers agreed in June 2025 to eliminate prior authorization for 12 common generic classes by January 2026. Federal and state reforms are accelerating. The Congressional Budget Office projects a 40% reduction in generic prior auth by 2028. The trend is clear: requiring approval for low-cost, proven generics is unsustainable, inefficient, and harmful.



8 Comments
Tony Du bled December 22, 2025 AT 21:45
So let me get this straight - we’re making people wait weeks for a $4 pill that’s been around since the 80s? This isn’t healthcare. It’s corporate theater with a side of bureaucratic slapstick.
Ajay Brahmandam December 23, 2025 AT 09:44
Been there. My dad’s on metformin and lisinopril. Got denied for both last month. Took 11 days. He missed two doses. His BP spiked. Doctor had to call in a favor with the pharmacy to get him a 3-day emergency supply. This system isn’t broken - it’s designed this way to bleed patients dry. And no one’s paying attention until it’s their mom’s thyroid med that gets stuck.
Johnnie R. Bailey December 23, 2025 AT 21:13
Here’s the ugly truth no one wants to say out loud: PBMs don’t care if you get your meds. They care if the generic you get pays them the biggest rebate. That’s why they push you from one $4 pill to another $4 pill - same active ingredient, same efficacy, different manufacturer, different kickback. It’s not clinical. It’s commerce disguised as cost control. And doctors? They’re stuck between a rock and a hard place - their time is being eaten alive by paperwork that serves zero medical purpose. The 17.3 hours per week stat? That’s not an outlier. That’s the norm. We’re not saving money. We’re just shifting the cost from the insurer’s balance sheet to the patient’s health - and the provider’s sanity.
And yeah, California’s law is a start. But until we break the rebate structure entirely - until we force PBMs to disclose every single dollar they make off these swaps - we’re just rearranging deck chairs on the Titanic. The goal shouldn’t be to approve generics. It should be to remove the entire approval layer. Let doctors prescribe. Let pharmacists dispense. Let patients heal.
Sam Black December 23, 2025 AT 21:59
I’ve watched my cousin’s husband sit in an ER for 18 hours because his insurance took 12 days to approve his atorvastatin. He had chest pain. They sent him home with a note saying "pending prior auth." He didn’t die. But he could’ve. And now he’s terrified to refill anything. This isn’t insurance. It’s a hostage situation with a form.
People talk about "clinical appropriateness" like it’s a noble cause. But when your doctor has to write a 3-page letter to justify giving you a drug that’s been in use since before you were born - that’s not medicine. That’s performance art for shareholders.
I work in a clinic. We have a binder labeled "Prior Auth Hell." It’s 3 inches thick. Half of it is for metformin. The other half? Lisinopril. Levothyroxine. Hydrochlorothiazide. All of them cheaper than a Starbucks latte. We don’t even joke about it anymore. We just sigh. And refill the coffee pot.
And yeah, the big insurers backing down in 2026? Good. But why did it take a federal law, state legislation, and a public outcry to make them do what they should’ve done in 2015? Because money talks. And patients? We’re just background noise.
I’m not mad. I’m just… tired. And I’m not alone.
Kathryn Weymouth December 24, 2025 AT 17:02
One thing people overlook: prior authorization delays don’t just affect patients. They affect providers’ mental health. I’ve had colleagues cry in the break room because they couldn’t get a patient’s levothyroxine approved in time, and the patient was showing signs of myxedema coma. The system isn’t just inefficient - it’s traumatizing. And yet, no one holds the PBMs accountable. They’re invisible. No CEO gives a speech about it. No news segment shows a family losing a loved one because their generic blood pressure med was stuck in a fax machine. We’ve normalized cruelty.
Julie Chavassieux December 25, 2025 AT 17:20
So now they’re making us beg for pills we’ve been taking for 10 years? Like we’re criminals? Like we’re trying to scam the system? I’m not trying to get high. I’m trying to stay alive. And now I have to jump through hoops just to get my metformin? What’s next? Do I need a background check to buy insulin? A psychological evaluation for my thyroid med? This is insane. And the worst part? No one cares until it’s their turn.
jenny guachamboza December 26, 2025 AT 08:09
THIS IS ALL A LIE. THEY’RE USING THIS TO TRACK US. THE PBMS ARE WORKING WITH THE GOVT TO PUT CHIPs IN OUR PILLS. METFORMIN ISN’T FOR DIABETES - IT’S A SURVEILLANCE TOOL. YOU THINK THEY’D LET YOU TAKE A $4 PILLS WITHOUT CONTROLLING YOU? HA. THEY WANT TO KNOW WHEN YOU TAKE IT. WHERE YOU ARE. HOW MUCH YOU’RE TAKING. IT’S ALL A COVER FOR MASS SURVEILLANCE. I SAW A VIDEO ON TIKTOK - A MAN GOT A PHONE CALL FROM HIS INSURER SAYING "WE NOTED YOUR 3AM METFORMIN DOSE. IS EVERYTHING OK?" THAT’S NOT COINCIDENCE. THAT’S A FEATURE. THEY’RE BUILDING A DATABASE. WE’RE ALL LAB RATS NOW.
Jamison Kissh December 28, 2025 AT 03:42
It’s funny - we built a system where the cheapest, safest, most effective treatments are the ones treated like contraband. We’ve inverted the entire logic of medicine. The more proven a drug is, the more suspicion it attracts. The more it’s used, the more hoops it has to jump through. It’s like the system is punishing success. Generics were supposed to be the triumph of science over greed. Now they’re the proof that greed learned how to mimic science. We’re not just fighting bureaucracy. We’re fighting the erosion of trust - in doctors, in insurers, in the idea that healthcare exists to heal, not to profit. And the saddest part? Most people don’t even notice until they’re the ones waiting for a pill that could’ve saved their life.