Those tiny stickers on your pill bottle aren’t just decoration-they’re lifesavers
You grab your prescription from the counter, toss the paper insert in the bag, and glance at the sticker on the bottle. Maybe you read it once. Maybe you didn’t. But that little piece of paper? It could be the difference between feeling better and ending up in the emergency room.
Every year, over 1.3 million people in the U.S. get hurt because of medication mistakes. Many of those mistakes happen because people don’t understand what the warnings on their bottles actually mean. The FDA requires these labels for a reason: they’re the last line of defense before a drug enters your body. And yet, only 55% of patients correctly interpret standard warning labels, according to the National Council on Patient Information and Education.
What the colors on your prescription label really mean
Not all warning stickers are created equal. The color isn’t random-it’s a quick visual cue designed to grab your attention based on risk level.
- Red means immediate danger. This is for things like "May cause severe liver damage" or "Do not take with alcohol". If you see red, stop and pay attention.
- Yellow means caution. These are warnings like "May cause drowsiness" or "Avoid sunlight". They’re not emergencies, but ignoring them can still lead to serious problems.
- Blue, white, or green are usually instructions, not warnings. Things like "Take with food" or "Refrigerate". Still important, but less urgent.
A 2017 study in U.S. Pharmacist found that 85% of patients correctly understood red labels as "danger," but only 45% understood blue ones the same way. That’s why red is reserved for the most serious risks-like Black Box Warnings.
Black Box Warnings: The FDA’s most serious alert
If your medication has a Black Box Warning, it’s the highest level of risk the FDA can assign. You’ll find it printed in bold, black borders on the drug’s official prescribing guide-and sometimes, it’s copied onto the label sticker too.
These warnings are added when a drug has been linked to life-threatening side effects. Examples include:
- Antidepressants: "May increase suicidal thoughts in young adults"
- Antibiotics like Cipro: "Risk of tendon rupture"
- Diabetes drugs like Avandia: "Increased risk of heart attack"
About 40% of new drugs approved between 2013 and 2017 carried a Black Box Warning, according to JAMA Internal Medicine. If your bottle has one, don’t skip the conversation with your pharmacist. This isn’t something you should guess your way through.

What "Take on empty stomach" really means
"Take on empty stomach" sounds simple. But what does it actually mean? Many people think it means "don’t eat right before." But the real rule is: at least one hour before or two hours after eating.
Why? Some drugs are absorbed poorly-or not at all-when food is in your system. For example:
- Antibiotics like amoxicillin work better without food
- Thyroid meds like levothyroxine can be blocked by calcium in dairy
- Some osteoporosis drugs like alendronate can cause serious stomach damage if taken with food
Same goes for "Take with food." That’s not just a suggestion-it’s often to protect your stomach. Drugs like ibuprofen or naproxen can cause ulcers if taken on an empty stomach. Food buffers the acid. Ignoring that warning isn’t bravery-it’s risky.
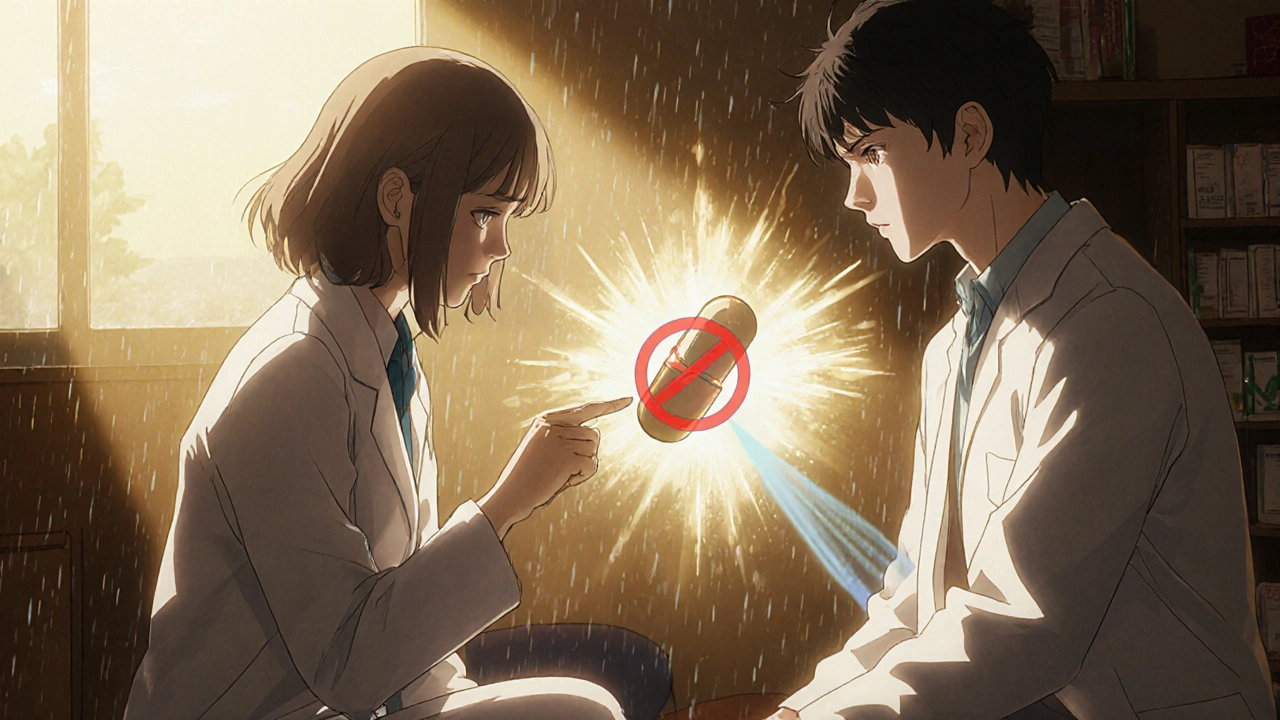
"Do not crush or chew"-and why people get it wrong
This warning is one of the most misunderstood. A 2022 Reddit thread from pharmacists showed that about 30% of patients think "do not crush or chew" means "chew it up so it dissolves faster." That’s the exact opposite of what it says.
Many pills are designed to release medicine slowly over time. Crushing them releases the full dose all at once. That’s dangerous:
- Crushing opioid painkillers like OxyContin can cause a fatal overdose
- Chewing extended-release stimulants like Adderall XR can send too much into your system too fast
- Some capsules have coatings to protect your stomach or delay absorption-crushing them ruins that
There’s now a universal "do not crush" symbol approved by the FDA in 2023. It looks like a pill with a red slash through it. In tests, this icon cut misinterpretation from 31% down to just 8%.
Why you’re ignoring the warnings (and how to stop)
It’s not just confusion-it’s habit. A Healthline survey found that 64% of people have ignored at least one warning. The top ignored ones?
- "Take with food" (42% ignored)
- "Avoid sunlight" (37% ignored)
- "Do not drink alcohol" (33% ignored)
Why? People think they know better. "I’ve taken this before and I’m fine." Or, "It’s just one time." But medications don’t always react the same way every time. Your liver changes. Your other meds change. Your body changes.
One patient on Drugs.com shared that she threw away the paper warning about grapefruit juice and her blood pressure med. She ended up in the ER with dangerously low blood pressure. Grapefruit juice interferes with over 85 drugs. It’s not a myth-it’s a known, dangerous interaction.
How to actually understand your labels (without a pharmacy degree)
You don’t need to be a doctor to read these warnings correctly. Here’s how to do it:
- Check the pill itself. Does the shape, color, and imprint match what’s on the label? If not, call the pharmacy. You might have the wrong drug.
- Look for color. Red = stop and ask. Yellow = be careful. White/blue = follow instructions.
- Ask the pharmacist to explain one warning. Don’t just say "What does this mean?" Say: "Can you explain the red sticker? I want to make sure I get it right."
- Use the "teach-back" method. After they explain, say: "So, if I take this with grapefruit juice, I could get dizzy and my blood pressure could drop too low. Is that right?" If they nod, you got it.
Studies show this simple trick improves understanding by 47%. It’s not just for elderly patients-it works for everyone.
What’s changing-and what you should expect soon
The system is finally starting to improve. In 2022, the FDA launched the "Facts Label" initiative, requiring simplified, easy-to-read medication guides for 20 high-risk drugs. By June 2025, all those labels must be redesigned using plain language and larger fonts.
Some pharmacies are testing QR codes on labels. Scan it, and you get a 60-second video explaining the warning in simple terms. Mayo Clinic trials showed this boosted understanding by over 50%.
By 2026, most pharmacies are expected to switch to standardized, evidence-based warning labels. Right now, only 37% use the best designs recommended by safety experts. That’s changing.
Don’t guess. Ask.
Prescription labels aren’t perfect. They’re often cluttered, confusing, and printed in tiny font. But they’re the best tool we have to prevent harm. The problem isn’t the labels-it’s how we treat them.
You wouldn’t ignore a warning sign on a construction site. Don’t ignore one on your pill bottle. If you’re unsure, call your pharmacy. Ask again. Say it out loud. Write it down. And if you’re still confused? Ask your doctor to explain it in person.
Medication safety isn’t about memorizing rules. It’s about asking questions. And that’s something you can do today-right now-before you swallow that next pill.



11 Comments
Conor McNamara November 18, 2025 AT 00:32
i swear the gov just puts these stickers so we feel like we're being watched. i once took my blood pressure med with grapefruit juice for 3 years and never got dizzy. now they want me to scan a qr code? lol. next they'll put a fingerprint scanner on the bottle.
steffi walsh November 18, 2025 AT 07:10
this is so important!! 🙌 i used to ignore the yellow ones until my mom had a bad reaction to her thyroid med because she took it with coffee. now i read every sticker like it's a love letter from my pharmacist. you guys are doing god's work 💙
Leilani O'Neill November 18, 2025 AT 09:03
I find it utterly pathetic that the average American needs color-coded stickers to understand basic pharmacology. In Ireland, we were taught in primary school that food interacts with drugs. This is why your healthcare system is a dumpster fire.
Riohlo (Or Rio) Marie November 19, 2025 AT 11:45
Let’s be real-the entire pharmaceutical-industrial complex is a glitter-coated scam. They don’t want you to understand the labels. They want you to feel obedient. The ‘black box’ isn’t a warning-it’s a velvet rope. And the QR codes? That’s just digital patting on the head while they keep raising your copay. 🤡
Girish Pai November 21, 2025 AT 08:40
In India, we have 12 different ways to take a single tablet depending on the season, moon phase, and whether your neighbor is angry. These US labels are child's play. Also, 'take with food' means eat chapati, not toast. Your buttered bread is ruining your statins.
Denny Sucipto November 21, 2025 AT 21:43
i used to crush my adderall because i thought it'd kick in faster. turns out i was basically doing a mini coke binge every morning. after my heart nearly exploded, i started asking my pharmacist to explain everything. now i feel like a genius for reading the tiny print. you guys are lifesavers 💪
Emanuel Jalba November 23, 2025 AT 12:22
THIS IS WHY AMERICA IS FALLING APART 😭 I saw a guy at CVS crush his OxyContin and snort it like a potato chip. I screamed. The pharmacist just shrugged. I cried in the parking lot. Someone please pass a law. I need to see justice. 🕊️💔
Heidi R November 24, 2025 AT 20:42
The fact that 64% ignore warnings proves most people are emotionally immature adults who think they’re immune to biology. Also, if you need a QR code to understand 'don’t drink alcohol with this,' maybe don’t have a prescription.
Gabe Solack November 26, 2025 AT 11:59
I used to roll my eyes at these stickers too... until my aunt had a stroke because she didn’t know grapefruit juice messed with her blood thinner. Now I print out the label info and tape it to my fridge. Took me 40 years to learn this. Don’t wait like I did. 🙏
Yash Nair November 26, 2025 AT 21:00
these warnings are just corporate propaganda. in india we use turmeric and holy basil for everything. why do you need a sticker to tell you not to drink with pills? its basic common sense. also your 'black box' is just a fancy way of saying 'we know this kills people but we still sell it'.
Bailey Sheppard November 28, 2025 AT 05:47
Honestly, the fact that we’re even having this conversation says more about our system than the labels do. But hey-this post made me call my pharmacist and ask about my new med. She smiled and said, 'Good for you.' Sometimes the simplest thing-asking-is the bravest.