Metformin Lactic Acidosis Risk Checker
Assess Your Risk
This tool estimates your risk of lactic acidosis based on key factors from FDA guidelines. It's not a medical diagnosis.
Risk Assessment Result
Metformin is the most common diabetes pill in the world
More than 150 million prescriptions for metformin are filled every year in the U.S. alone. It’s cheap, effective, and often the first drug doctors reach for when someone is diagnosed with type 2 diabetes. But for all its benefits, it comes with two big concerns that scare people: stomach problems and a rare but deadly condition called lactic acidosis. You don’t need to avoid metformin - but you do need to understand what’s normal and what’s dangerous.
Stomach issues are common - but usually temporary
About 1 in 3 people who start metformin get digestive trouble. Diarrhea is the most frequent complaint, hitting more than half of those affected. Nausea, stomach cramps, vomiting, and loss of appetite are also common. These aren’t allergies or signs of something seriously wrong. They’re just how your body reacts to the drug at first.
Most of these symptoms show up in the first 30 days. A study tracking 7,430 people found that 68% felt sick within the first month. But here’s the good news: 85% of those people saw their symptoms fade within 2 to 4 weeks. This isn’t something you have to live with forever.
What helps? Start low and go slow. Many people feel better when they begin with a 500 mg dose once a day, usually with dinner. If that’s tolerable, they slowly increase the dose over weeks. Switching to an extended-release version (metformin ER) cuts stomach problems by nearly half. One patient on Reddit said switching to 500 mg ER at night dropped their diarrhea from 4-5 times a day to just occasional cramps - within 10 days.
Take metformin with food. Don’t take it on an empty stomach. Avoid high-fat meals right after dosing - they can make nausea worse. If you’re still struggling after a month, talk to your doctor about switching formulations or adjusting timing. Don’t quit cold turkey. Stopping abruptly can cause blood sugar spikes.
Lactic acidosis is rare - but deadly
Lactic acidosis is the reason metformin carries a black box warning from the FDA. It’s the most serious side effect. But you need to understand how rare it really is.
Out of 15.2 million metformin users in 2022, only 12 confirmed cases of lactic acidosis were reported. That’s 0.079 cases per 100,000 people. For comparison, you’re more likely to be struck by lightning than to get metformin-associated lactic acidosis (MALA) if you’re healthy and taking the drug as prescribed.
But when it does happen, it’s dangerous. About 30-50% of people who develop MALA die from it. That’s why you need to recognize the warning signs fast:
- Extreme fatigue - almost everyone with MALA feels this
- Rapid, shallow breathing
- Nausea or vomiting that won’t go away
- Stomach pain or muscle aches
- Feeling unusually cold or having cold skin
If you have any of these, especially together, go to the ER. Don’t wait. Lactic acidosis is confirmed with blood tests: arterial pH below 7.35, lactate above 5 mmol/L, and an anion gap over 12. These aren’t numbers your doctor checks routinely - they’re tested when you’re already showing symptoms.

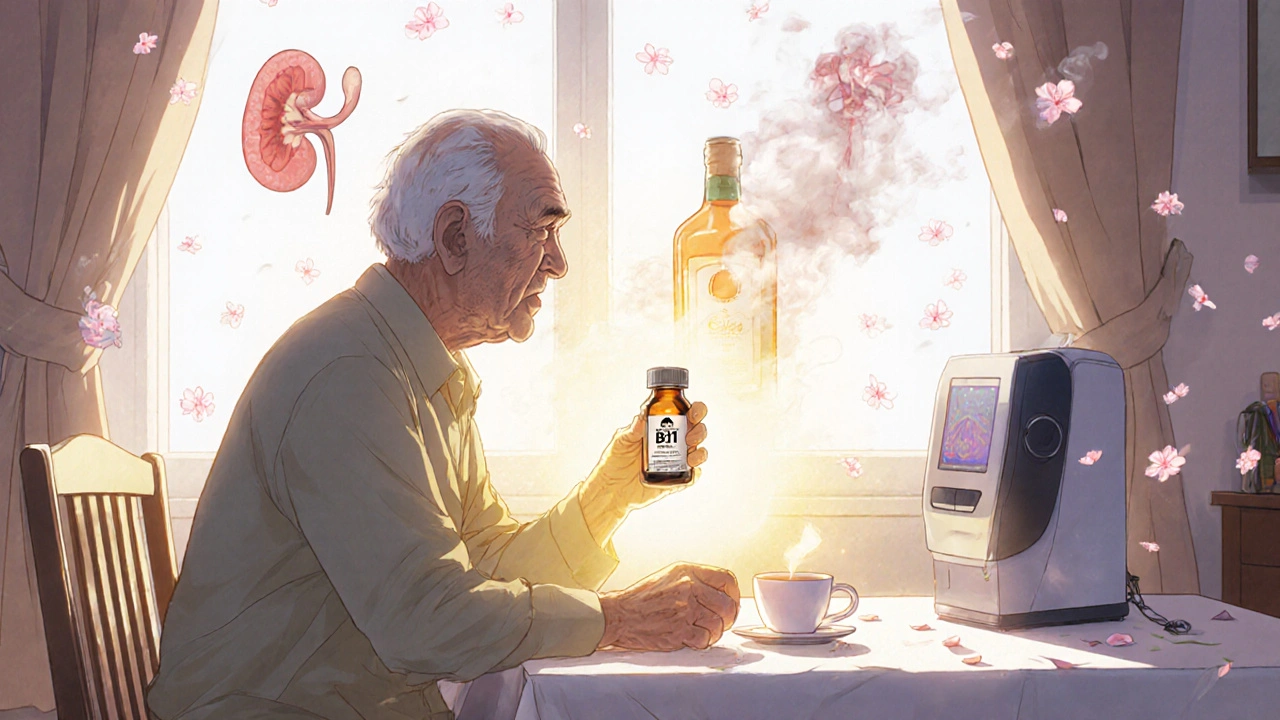
Who’s at real risk for lactic acidosis?
The biggest myth about metformin is that it causes lactic acidosis in healthy people. It doesn’t. Almost all cases happen in people with serious health problems.
Here are the real risk factors:
- Severe kidney disease: If your eGFR is below 30, you’re 18.7 times more likely to develop MALA. That’s why doctors stop metformin at this level.
- Acute kidney injury: A sudden drop in kidney function - from dehydration, infection, or heart failure - raises risk 24 times.
- Liver failure: Your liver helps clear lactate. If it’s damaged, risk goes up 8 times.
- Age over 80: Older bodies process drugs slower. Risk increases nearly 5 times.
- Heavy alcohol use: Drinking 3 or more drinks a day raises risk nearly 7 times.
Doctors check your kidney function every 3 to 6 months if your eGFR is between 45 and 59. If it’s below 45, they check monthly. If your creatinine is above 1.4 mg/dL (men) or 1.1 mg/dL (women), metformin is not safe to use.
Before any procedure that uses contrast dye (like a CT scan), you’ll be told to stop metformin 48 hours before and after. This is standard. It’s not because the dye causes lactic acidosis - it’s because the dye can temporarily hurt your kidneys. And if your kidneys slow down while you’re on metformin, lactate builds up.
What metformin doesn’t do
There’s a lot of fear around metformin. Some people think it damages kidneys, causes dementia, or permanently lowers vitamin B12. None of that’s true.
Metformin doesn’t hurt your kidneys. It doesn’t cause kidney disease. In fact, studies show it has no effect on kidney function over 10 years. If your kidneys fail while you’re on metformin, it’s because of something else - diabetes, high blood pressure, or another illness.
It doesn’t cause dementia. One large study found no link between metformin use and memory loss or Alzheimer’s. Some research even suggests it might help protect the brain.
It can lower B12 - but it’s fixable. About 7% of people on metformin long-term have lower B12 levels. This isn’t permanent. It’s easily reversed with over-the-counter B12 supplements. The American Association of Clinical Endocrinologists now recommends checking B12 every year if you’ve been on metformin for more than 4 years.
New options are coming
In May 2023, the FDA approved a new version of metformin called Metformin-ER-XR. In clinical trials, it caused 42.7% fewer stomach problems than the old extended-release formula. If you’ve struggled with GI side effects for years, this might be worth asking your doctor about.
There’s also a big NIH-funded study called TAME (Targeting Aging with Metformin) that’s testing whether metformin can delay aging-related diseases. But don’t start taking it just because you want to live longer. There’s no proof yet that it works for that - and using it without diabetes can be risky.
Bottom line: Metformin is safe if you’re monitored
Metformin isn’t perfect. But it’s the best tool we have for managing type 2 diabetes for most people. The stomach issues? Usually go away. The lactic acidosis risk? Extremely low if you’re healthy and your kidneys work fine.
Here’s what you should do:
- Start with the lowest dose and increase slowly.
- Take it with food, preferably dinner.
- Ask about the extended-release version if you have stomach problems.
- Get your kidney function checked every 3-6 months.
- Stop metformin before any imaging with contrast dye.
- Call your doctor or go to the ER if you feel extreme fatigue, trouble breathing, or severe nausea with muscle pain.
- Get your B12 checked yearly after 4 years of use.
Don’t let fear stop you from taking a drug that’s helped millions control their blood sugar, lose weight, and avoid complications. Just be smart about it. Know your risks. Know your body. And talk to your doctor - not Google.
Does metformin cause permanent stomach damage?
No. Metformin does not cause permanent damage to the stomach or intestines. Gastrointestinal side effects like diarrhea, nausea, and cramping are temporary and usually resolve within 2 to 4 weeks. Switching to an extended-release formulation or adjusting the timing of doses often eliminates these issues completely.
Can I take metformin if I have mild kidney disease?
Yes, but with caution. If your eGFR is between 30 and 45 mL/min/1.73m², your doctor may reduce your dose or monitor you more closely. Metformin is not recommended if your eGFR drops below 30. Regular kidney tests are required - usually every 3 to 6 months - to ensure safety.
Is lactic acidosis from metformin common in healthy people?
No. Lactic acidosis from metformin is extremely rare in healthy individuals with normal kidney and liver function. Almost all cases occur in people with serious underlying conditions like kidney failure, liver disease, heart failure, or severe infection. The drug itself doesn’t cause it in otherwise healthy users.
Should I stop metformin if I get the flu or a stomach bug?
Yes, temporarily. If you’re severely dehydrated, vomiting, or unable to eat due to illness, your risk of lactic acidosis increases. Stop metformin until you’re back to normal and hydrated. Talk to your doctor about when to restart it. Do not restart without medical advice.
Does metformin cause weight loss?
Yes, modestly. Many people lose 2 to 5 pounds on metformin, especially in the first few months. It helps reduce appetite and may improve how your body uses insulin. It’s not a weight-loss drug, but the effect is real and often helpful for people with type 2 diabetes who are overweight.
Can I drink alcohol while taking metformin?
Occasional light drinking is usually safe. But heavy alcohol use (3 or more drinks per day) increases your risk of lactic acidosis by nearly 7 times. Alcohol affects the liver and can lower blood sugar. If you drink regularly, talk to your doctor about safer limits.
How long does it take for metformin to start working?
You may notice lower blood sugar in 1 to 2 weeks, but it can take up to 2 to 3 months to reach full effect. Don’t expect instant results. Consistency matters more than dosage spikes. Take it as prescribed, even if you feel fine.
What should I do if I miss a dose?
If you miss a dose, take it as soon as you remember - unless it’s close to your next scheduled dose. Never double up. Missing one dose won’t cause a spike, but consistently skipping doses can make your blood sugar harder to control. Set phone reminders if needed.



13 Comments
Bruce Bain November 19, 2025 AT 02:40
I started metformin last year and thought I was gonna die from the diarrhea. Then I switched to ER and took it with dinner. Boom. No more 5x-a-day runs. Just a little gurgle now and then. Life's good.
Don Angel November 19, 2025 AT 02:41
I'm so glad someone finally broke this down without scare tactics. Seriously, people panic over lactic acidosis like it's a horror movie. You're more likely to get hit by a vending machine than get MALA if you're not a walking emergency. Just get your kidneys checked. That's it.!!!
benedict nwokedi November 20, 2025 AT 17:02
Let me guess - the pharmaceutical industry paid the FDA to downplay the real danger. Lactic acidosis isn't 'rare' - it's covered up. They don't want you to know that metformin is just a cheap, slow-acting poison that mimics starvation. Your liver is being suffocated while you're told to 'take it with food.' And don't get me started on the B12 scam - they know you'll get neuropathy and then sell you supplements. It's all a cycle. Don't be fooled.
deepak kumar November 21, 2025 AT 19:34
I'm from India and metformin is like water here - everyone takes it. My uncle had stomach issues for 3 weeks, then switched to ER. Now he's hiking at 70. Kidney checks? Yes. B12? Yes. Alcohol? Rarely. Simple. No drama. Just science. You got this.
Dave Pritchard November 22, 2025 AT 11:33
If you're reading this and scared - breathe. You're not alone. A lot of people feel like they're about to explode from GI issues at first. But it's not your body rejecting the drug - it's just learning. Slow down. Talk to your doc. Try ER. You'll be fine. I've seen it a hundred times.
kim pu November 24, 2025 AT 05:11
Okay but what if I told you metformin is just a beta-blocker in disguise? They gave it to diabetics because it 'lowers insulin resistance' - but really it's just suppressing your sympathetic nervous system so you don't feel the stress of eating carbs. And the 'B12 deficiency'? That's the body's way of screaming for help. They want you dependent on supplements. Wake up.
malik recoba November 24, 2025 AT 20:02
i was so scared to start metformin after reading online. i thought i’d be puking every day. i took the 500mg with dinner and just waited. after 2 weeks it was like nothing. my stomach is fine now. i just forgot to take it once and my sugar went up. so yeah, consistency matters. thanks for the post!
Sarbjit Singh November 25, 2025 AT 06:47
Bro, metformin ER changed my life 😊 I used to run to the bathroom 6x a day. Now? Maybe once. And my A1C dropped from 8.2 to 6.1. Keep going, you got this! 💪
Angela J November 27, 2025 AT 05:42
I don't trust this. The CDC knows metformin causes mitochondrial damage. They just don't tell you because they're afraid of lawsuits. And why do they say 'rare'? Because they only count the ones who die in hospitals. What about the ones who get chronic fatigue and are just told to 'take vitamins'? That's not rare - that's a cover-up.
Sameer Tawde November 27, 2025 AT 05:57
Start low. Take with food. Use ER. Check kidneys yearly. Done. No magic. Just smart. You're not broken. You're managing. Keep going.
Jeff Hakojarvi November 27, 2025 AT 18:55
I had a patient who stopped metformin cold turkey because she read a blog about lactic acidosis. Her A1C jumped to 11. She ended up in the ER with DKA. Don't quit because of fear. Talk to your provider. Adjust. Don't abandon. You're worth the effort.
Timothy Uchechukwu November 27, 2025 AT 19:21
In Nigeria we don't have this problem because we don't overmedicate. People here eat real food and walk everywhere. Metformin is a Western crutch. You don't need pills if you stop eating sugar and sit less. This whole thing is a scam to sell drugs to lazy people
Ancel Fortuin November 28, 2025 AT 16:01
So... you're telling me the FDA is trustworthy now? After everything? And you believe a study that says 'only 12 cases'? What if they only reported 12 out of 1200? What if the real number is buried under 'gastroenteritis' or 'unspecified acidosis'? I don't trust the numbers. I trust my gut. And my gut says this is all a lie.