When you’re pregnant and managing a mental health condition, the question isn’t just whether to take medication-it’s how to decide, with confidence, and without fear. Too many people are told to stop their meds cold turkey the moment they find out they’re pregnant. Others are handed a prescription with no real talk about risks. Neither approach works. The truth is, there’s no risk-free choice. But there is a better way: shared decision-making.
Why Stopping Meds Isn’t Always Safer
It’s a common myth that avoiding medication during pregnancy automatically means a safer baby. But untreated depression, anxiety, or bipolar disorder carries real, measurable risks. Studies show that pregnant people with unmanaged depression are 30% to 50% more likely to have a preterm birth. The risk of miscarriage, low birth weight, and developmental delays also rises. And the emotional toll on the parent? It’s devastating. One in five people with untreated perinatal depression will have suicidal thoughts. That’s not a small number-it’s a crisis. The real danger isn’t always the medicine. It’s the silence around it. A 2023 survey found that 68% of pregnant people felt they weren’t properly informed about their medication options before getting pregnant. Nearly half stopped their meds on their own because they were scared of birth defects. And when they did, many ended up worse off-hospitalized, overwhelmed, or relapsing into severe depression or psychosis.What Shared Decision-Making Actually Looks Like
Shared decision-making isn’t just a fancy phrase. It’s a process. It means you and your provider sit down, look at real numbers, and make a plan together. No pressure. No judgment. Just facts. Here’s how it works in practice:- You talk about your history: How long have you been on medication? Have you relapsed before? How severe were your symptoms?
- Your provider shares the data: What’s the actual risk of birth defects with your specific drug? How likely is it that stopping will lead to a relapse?
- You both weigh the trade-offs: Is the risk of a 2 in 1,000 chance of heart defect worth the 80% chance you’ll fall into severe depression again?
- You make a plan-with a backup.
Which Medications Are Actually Safe?
Not all psychiatric meds are created equal. Some have decades of safety data. Others? Not so much. SSRIs-like sertraline (Zoloft), citalopram (Celexa), escitalopram (Lexapro), and fluoxetine (Prozac)-are the most studied and generally recommended as first-line during pregnancy. They don’t increase the risk of major birth defects in most cases. The exception? Paroxetine (Paxil). It’s linked to a slightly higher chance of heart defects-about 1 in 100 births instead of the usual 8 in 1,000. That’s why most providers avoid it unless absolutely necessary. For bipolar disorder, lamotrigine is often the go-to. It doesn’t cause major birth defects, unlike valproic acid (Depakote), which can increase the risk of neural tube defects from 0.1% to 1-2%. That’s a 10-to-20 times higher risk. If you’re on valproic acid and planning pregnancy, switching before conception is critical. Lithium is another option for bipolar, but it requires close monitoring. Your body changes during pregnancy-your kidneys process it differently. Doses often need to be adjusted, and your levels must be checked weekly in the third trimester. Bupropion (Wellbutrin) is sometimes used, especially if SSRIs don’t work or cause side effects. But it’s linked to a small increase in miscarriage and heart defects. Still, for some, the benefits outweigh the risks. And for psychosis? Typical antipsychotics like haloperidol and chlorpromazine have been around longer and have better safety data. Atypical antipsychotics like risperidone or quetiapine? Less clear. Long-term child outcomes aren’t well studied yet. That’s why many providers avoid them unless there’s no other choice.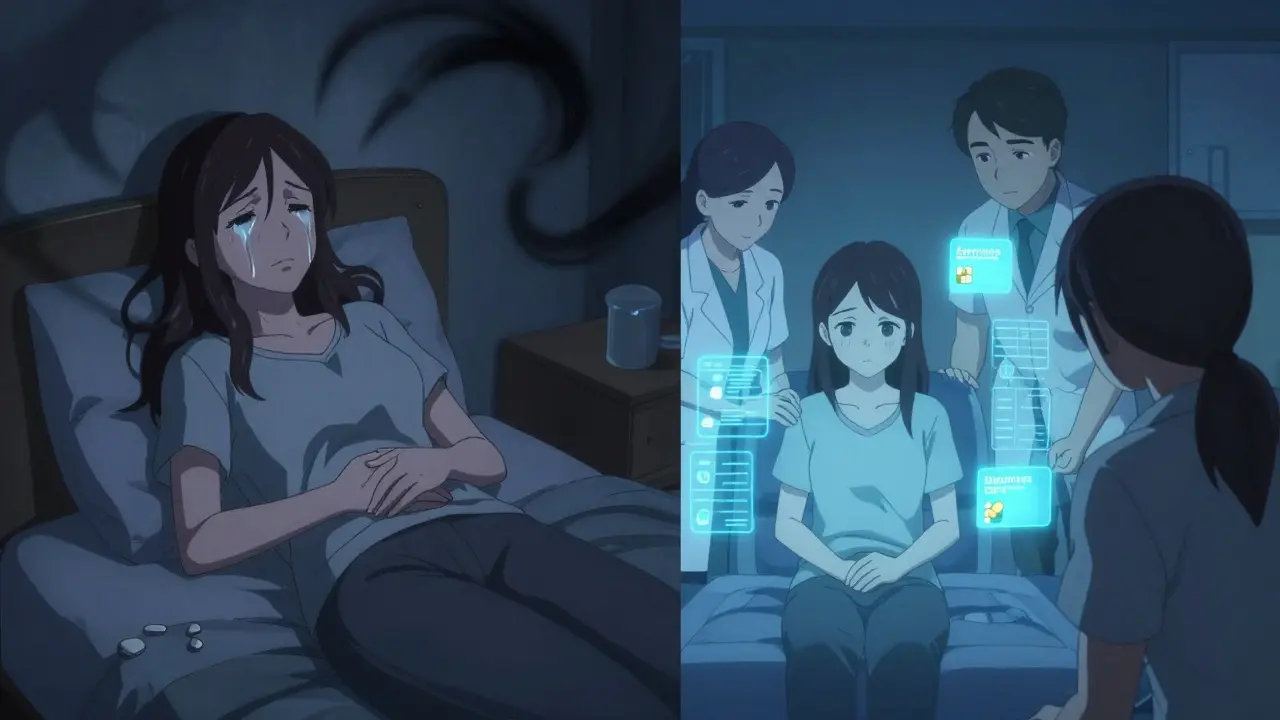
The Numbers Behind the Fear
Fear often comes from vague warnings: "This drug might cause problems." But what does "might" mean? Here’s what the data actually says:- SSRIs: 1.5 times higher odds of having a baby smaller than expected for gestational age. That’s a real concern, but not a deal-breaker.
- Paroxetine: 1.28 times higher odds of heart defects in the first trimester. That’s a 2% risk instead of 1.6%.
- Untreated depression: 30-50% higher risk of preterm birth. That’s a bigger risk than most meds.
- Relapse after stopping meds: Up to 80% for people with severe depression.
What Experts Are Saying
Dr. Lee Cohen, who runs the National Pregnancy Registry for Psychiatric Medications, puts it bluntly: "The risk of stopping treatment often outweighs the risk of the medication." His registry has tracked over 15,000 pregnancies since 2010. The data shows that people who stayed on their meds and were monitored closely had better outcomes than those who stopped. The University of Washington’s Perinatal Clinical Liaison service has a simple rule: "If you’re thinking of stopping your patient’s meds because they’re pregnant-call us first." Why? Because stopping doesn’t eliminate risk. It just swaps one kind of risk for another. And Dr. Samantha Meltzer-Brody, who helped write the 2023 ACOG guidelines, says: "If you can stabilize your mental health for at least three months before getting pregnant, your chance of relapse drops by 40%." That’s why preconception planning isn’t optional-it’s essential.Tools That Actually Help
The ACOG-endorsed Mental Health Medication Decision Aid is one of the few tools that gives real, up-to-date numbers for 24 different medications. It’s updated quarterly with data from the National Pregnancy Registry. Providers should use it-not just to inform, but to document the conversation. You can also ask for tools like the Edinburgh Postnatal Depression Scale to track your mood over time. If your score is above 10, you’re at higher risk for relapse. That’s a red flag that your meds might need adjusting. And here’s something most people don’t know: documenting this conversation reduces malpractice claims by 65%. Why? Because when you’ve had a real, documented discussion, there’s no guesswork. You and your provider are on the same page.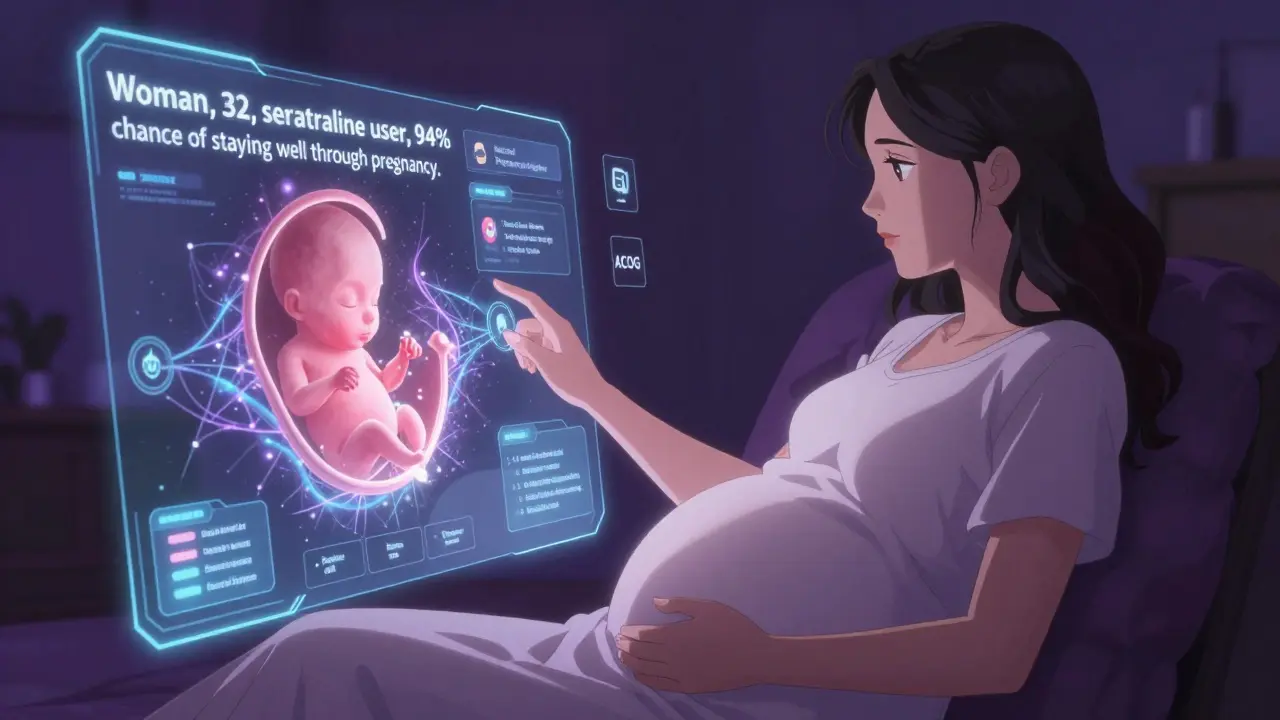
What You Can Do Right Now
If you’re pregnant or thinking about it:- Don’t stop your meds without talking to your provider. Even if you’re scared.
- Ask for the decision aid. If your provider doesn’t have it, ask where to find it.
- Get your mental health stable before conception if you can. Even three months of stability makes a difference.
- Find a perinatal psychiatrist. 87% of OB-GYNs now consult them. You don’t have to do this alone.
- Join a support group. Reddit’s r/PostpartumDepression has 125,000 members. You’re not the only one feeling this way.
What’s Changing in 2026
The field is moving fast. By 2026, shared decision-making tools will use real-time data from the National Pregnancy Registry to give you personalized risk estimates-not just population averages. Imagine this: you’re 32, have a history of severe depression, took sertraline for two years, and now you’re pregnant. The tool doesn’t say "SSRIs have a 1.5% risk." It says, "Women like you who stayed on sertraline had a 1.2% risk of preterm birth and a 94% chance of staying well through pregnancy." That’s not science fiction. It’s coming. And the cost-benefit? Every dollar spent on shared decision-making saves $4.70 in avoided hospital stays, NICU care, and long-term developmental support. That’s not just good medicine. It’s smart policy.Final Thought
You don’t have to choose between being a good mom and being mentally well. You can be both. But you need the right information, the right support, and the right conversation. This isn’t about fear. It’s about agency. You deserve to make a choice that’s informed, personal, and respected.Are SSRIs safe during pregnancy?
Yes, most SSRIs like sertraline, citalopram, and escitalopram are considered safe and are first-line treatments during pregnancy. They have the most safety data and are not linked to major birth defects, except for paroxetine, which carries a slightly higher risk of heart defects. The benefits of treating depression often outweigh the small risks.
Can I breastfeed while taking mental health meds?
Yes, most SSRIs and lamotrigine pass into breast milk in very small amounts and are considered compatible with breastfeeding. Sertraline is often preferred because it has the lowest levels in breast milk. Always discuss your specific medication with your provider, but stopping meds to breastfeed is rarely necessary or recommended.
What if I’m on lithium or valproic acid?
Lithium requires close monitoring during pregnancy because your body processes it differently-it can build up and affect the baby’s heart. Valproic acid is strongly discouraged because it increases the risk of neural tube defects and autism. If you’re on either, talk to your provider before getting pregnant. Switching to a safer option like lamotrigine is often possible and recommended.
Is it true that stopping meds increases the risk of relapse?
Yes. Studies show that 80% of people with severe depression relapse during pregnancy if they stop their meds. That’s higher than the risk of birth defects from most medications. Untreated depression also raises the risk of preterm birth, low birth weight, and postpartum psychosis.
How do I find a perinatal psychiatrist?
Ask your OB-GYN for a referral. Many hospitals have perinatal psychiatry programs. You can also search through the National Pregnancy Registry for Psychiatric Medications or contact Postpartum Support International. They can connect you with specialists who understand both pregnancy and mental health.



10 Comments
laura Drever January 13, 2026 AT 13:47
ive been on zoloft for 5 years and got pregnant last year i just stopped cold turkey because everyone kept saying its dangerous now im crying every day and my baby is 3 months old and i feel like a failure
Randall Little January 14, 2026 AT 13:15
Oh wow. So we’re just supposed to trust the data now? Next you’ll tell me the sun doesn’t rise because quantum physics says it’s an illusion. Let me guess-your OB-GYN also reads peer-reviewed journals in bed while sipping kombucha?
jefferson fernandes January 14, 2026 AT 20:41
Look. I get it. You're scared. But this isn't about fear-it's about facts. SSRIs like sertraline? Safe. Paroxetine? Avoid. Lithium? Monitor like crazy. Valproate? Don't even think about it unless you want a child with a 2% chance of spina bifida. This isn't opinion. This is medicine. And if your provider isn't walking you through this step-by-step, find a new one. Your mental health isn't optional. Neither is your baby's safety. You deserve both.
lucy cooke January 15, 2026 AT 15:57
Oh darling, it's not just about medication-it's about the soul's quiet scream in a world that tells you to be quiet. We're told to swallow pills like they're candy, then blamed when we cry. But what if the real illness isn't depression? What if it's a society that demands perfection from broken women? I'm not just talking about SSRIs-I'm talking about the silence. The shame. The way we're taught to choose between being a 'good mother' and being human. I weep for us.
John Tran January 17, 2026 AT 03:12
So let me get this straight-you’re telling me that if I’m on lamotrigine and I get pregnant, I shouldn’t panic because it’s ‘safe’? But then what about the 2021 study from the Lancet that showed a slight increase in cleft palate when combined with polypharmacy? And what about the fact that most of this data comes from white, middle-class women in the US? What about the immigrant moms in rural Texas who don’t speak English and are handed a script with no translation? Or the ones who can’t afford to see a perinatal psychiatrist because their insurance won’t cover it? This isn’t just science-it’s privilege wrapped in a white coat. And until we fix that, ‘shared decision-making’ is just corporate jargon for ‘good luck.’
Pankaj Singh January 18, 2026 AT 04:39
Stop being dramatic. If you can’t handle your mental illness without drugs, you shouldn’t be having kids. End of story.
Robin Williams January 18, 2026 AT 13:42
Bro. I was on prozac during my pregnancy. I didn’t stop. I didn’t panic. I just kept living. And guess what? My kid is 7 now and plays piano and loves dinosaurs. Mental health isn’t a weakness. It’s a part of you. And if you’re scared? Talk to someone. Not Reddit. Not your aunt. A real doc. You got this.
Angel Molano January 20, 2026 AT 12:51
You’re not a victim. You’re a choice. If you take drugs while pregnant, you’re choosing to risk your child’s life. No excuses.
James Castner January 21, 2026 AT 08:55
It is imperative that we recognize the profound ethical and clinical dimensions of perinatal psychiatric care. The data presented herein, derived from longitudinal, peer-reviewed, multi-center registries, demonstrates unequivocally that the risk-benefit calculus favors continued pharmacological management in the majority of clinically significant cases. To suggest otherwise is not only medically unsound-it is ethically indefensible. Furthermore, the socioeconomic disparities in access to perinatal psychiatry represent a systemic failure of public health infrastructure, and must be addressed with urgency, equity, and institutional accountability. We must not reduce complex human experiences to binary choices. Agency requires knowledge. Knowledge requires access. Access requires justice.
Adam Rivera January 21, 2026 AT 18:50
Hey, I’m a dad and my wife was on Lexapro during her pregnancy. We used the decision aid tool you mentioned. It helped us feel less alone. If you’re reading this and scared-reach out. You’re not broken. You’re brave. And you’re not doing this alone.