Macrolide Antibiotic Risk Calculator
Personal Risk Assessment
This tool helps assess your individual risk of QT prolongation when taking macrolide antibiotics based on key factors identified in medical research.
When you take an antibiotic like azithromycin or clarithromycin for a sinus infection or pneumonia, you’re probably not thinking about your heart. But for some people, these common drugs can trigger a dangerous change in heart rhythm - one that can be life-threatening. The issue isn’t rare, and it’s not theoretical. It’s documented in medical journals, flagged by the FDA, and tracked by hospitals across the U.S. The problem? QT prolongation.
What Is QT Prolongation, and Why Does It Matter?
Your heart beats because of electrical signals that move through muscle tissue in a precise sequence. The QT interval on an ECG measures how long it takes for the heart’s lower chambers to recharge between beats. If that interval gets too long, your heart can slip into a chaotic rhythm called Torsades de Pointes - a type of ventricular tachycardia that can turn into sudden cardiac arrest. Macrolide antibiotics like azithromycin, clarithromycin, and erythromycin interfere with a key potassium channel in heart cells (called hERG). This blocks the flow of potassium out of the cell during repolarization, slowing down the heart’s recovery phase. The result? A longer QT interval. It doesn’t happen in everyone. But when it does, the consequences can be sudden and severe.Not All Macrolides Are the Same
You might think all macrolides carry the same risk. They don’t. The cardiac danger varies significantly between them. Clarithromycin has the highest risk. It doesn’t just block potassium channels - it also strongly inhibits CYP3A4, a liver enzyme that breaks down many other drugs. This means if you’re taking clarithromycin along with a statin, blood pressure med, or even an antifungal, those drugs can build up in your system and push your QT interval even higher. The FDA requires a black box warning on clarithromycin labels for this reason. Erythromycin is less potent at blocking potassium channels than clarithromycin, but it’s notorious for causing nausea and vomiting. That can lead to low potassium levels - a major trigger for arrhythmias. So even if its direct effect on the heart is weaker, its side effects make it just as dangerous in practice. Azithromycin was once considered the safest option. It barely affects CYP3A4 and has weaker potassium channel blockade. But in 2012, a landmark study of over 1.3 million patients found that azithromycin was linked to a 2.85-fold increase in cardiovascular death within the first five days of use compared to amoxicillin. That’s not a small number. The FDA added a warning to its label, though not a black box. Still, azithromycin accounts for 65% of all macrolide prescriptions in the U.S. - and that’s because many doctors still believe it’s low-risk.Who’s Most at Risk?
The good news? Most healthy people won’t have a problem. The bad news? If you have even one risk factor, your chance of trouble jumps dramatically. Here are the six biggest red flags:- Female sex: Women make up nearly 70% of documented TdP cases. Hormonal differences and slower drug metabolism play a role.
- Age 65 or older: The risk doubles. Aging hearts are less able to compensate for electrical disruptions.
- Baseline QTc over 450 ms: If your ECG already shows a prolonged interval, macrolides can push you into danger zone territory.
- Other QT-prolonging drugs: Taking two or more drugs that affect the QT interval - like antidepressants, antifungals, or antiarrhythmics - multiplies your risk. Each extra drug adds about 80% more danger.
- Low potassium or magnesium: Hypokalemia increases risk over threefold. This is why dehydration or diuretics can turn a safe prescription into a cardiac emergency.
- Heart failure or structural heart disease: Your heart is already strained. Adding a drug that disrupts its rhythm? That’s a recipe for disaster. Risk increases over fivefold.
And here’s something many doctors miss: You can have a normal ECG and still be at risk. Some people carry silent gene mutations in their hERG channels - a condition called congenital long QT syndrome. It doesn’t show up until a drug like azithromycin triggers it. Family history of sudden cardiac death before age 50? That’s a red flag.
When Should You Get an ECG?
You don’t need an ECG before every antibiotic. But if you have two or more risk factors, ask for one. The American College of Cardiology recommends baseline ECG testing for patients with:- Age over 65
- History of heart disease
- Use of other QT-prolonging medications
- Electrolyte imbalances
After starting the antibiotic, get a repeat ECG if your QTc goes above 470 ms in men or 480 ms in women - or if it increases by more than 60 ms from your baseline. That’s the threshold experts use to decide whether to stop the drug.
What Should You Do If You’re Prescribed a Macrolide?
If you’re healthy and under 65 with no heart issues and no other medications, azithromycin is still a reasonable choice for most infections. But here’s what to do if you’re in a higher-risk group:- Ask your doctor: “Is there a non-macrolide alternative?” Amoxicillin, doxycycline, or cephalexin are often just as effective for respiratory infections.
- Don’t take macrolides if you’ve had TdP before - they’re absolutely contraindicated.
- Get your potassium levels checked if you’re on diuretics or have had vomiting/diarrhea.
- Don’t combine macrolides with antifungals, antidepressants, or heart rhythm drugs unless your doctor has reviewed all your meds.
- If you feel dizzy, faint, or have palpitations while on the drug - stop it and get help immediately.
What’s Changing in 2026?
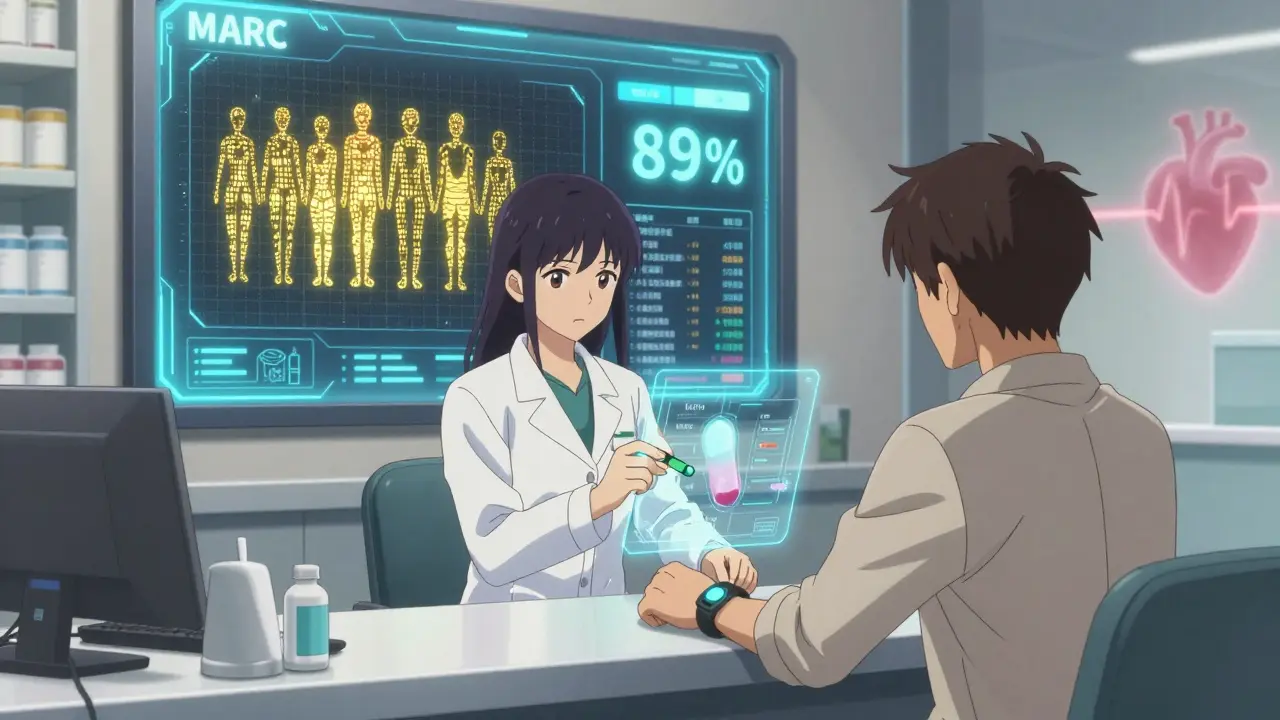
The field is evolving fast. In 2023, the FDA approved a new handheld ECG device called the CardioCare QT Monitor that gives accurate QTc readings in under 30 seconds. Emergency rooms and clinics are starting to use it to screen patients before prescribing macrolides. A new tool called the Macrolide Arrhythmia Risk Calculator (MARC) is being rolled out in major hospitals. It takes 12 inputs - age, sex, meds, labs, ECG, family history - and gives you a personalized risk score. In validation studies, it predicted TdP with 89% accuracy. Researchers are also working on “cardiosafe” macrolides. One candidate, solithromycin, showed 78% less potassium channel blockade than clarithromycin. Unfortunately, it was pulled from development in 2022 due to liver toxicity. But the work continues. Meanwhile, the NIH is funding studies to find genetic markers that make people more sensitive to macrolide-induced QT prolongation. Early data suggests 15% of the population carries variants that increase their risk over fourfold. Imagine a future where your pharmacist runs a quick genetic check before filling your antibiotic prescription.Bottom Line: Know Your Risk, Ask Questions
Macrolide antibiotics are powerful tools. But they’re not harmless. The risk of a fatal arrhythmia is low for most people - but it’s not zero. And for those with even one risk factor, the danger becomes real. If you’re prescribed azithromycin, clarithromycin, or erythromycin, don’t assume it’s safe just because it’s common. Ask your doctor: Do I have any risk factors? Should I get an ECG? Is there a safer alternative? Your heart doesn’t always warn you before it stumbles. But with the right questions, you can help prevent the fall.Can azithromycin really cause heart rhythm problems?
Yes. While azithromycin has a lower risk than clarithromycin or erythromycin, studies show it can still prolong the QT interval and trigger Torsades de Pointes, especially in people with risk factors like older age, female sex, low potassium, or existing heart disease. A 2012 study found a 2.85-fold increase in cardiovascular deaths during the first five days of use compared to amoxicillin.
Which macrolide antibiotic is safest for the heart?
Azithromycin carries the lowest cardiac risk among macrolides because it has minimal effect on the CYP3A4 enzyme and weaker potassium channel blockade. However, no macrolide is completely safe. Even azithromycin can be dangerous in high-risk patients. For people with multiple risk factors, non-macrolide antibiotics like amoxicillin or doxycycline are often better choices.
How do I know if my QT interval is prolonged?
You need an ECG. The corrected QT interval (QTc) is measured on a standard electrocardiogram. A QTc over 450 ms in men or 470 ms in women is considered prolonged. If it’s over 500 ms or increases by more than 60 ms from baseline, the risk of dangerous arrhythmias rises sharply. Don’t rely on symptoms - many people feel fine until it’s too late.
Should I avoid macrolides if I’m on other medications?
Yes, if those other medications also prolong the QT interval. Common ones include certain antidepressants (like citalopram), antifungals (like fluconazole), antiarrhythmics (like amiodarone), and even some antihistamines. Combining them with macrolides can push your QT interval into dangerous territory. Always tell your doctor or pharmacist about every medication you take - including over-the-counter and herbal supplements.
What should I do if I feel dizzy or have palpitations while taking a macrolide?
Stop taking the antibiotic immediately and seek medical attention. Dizziness, fainting, or irregular heartbeat could be signs of Torsades de Pointes. This is a medical emergency. Don’t wait to see if it passes. Call 911 or go to the nearest emergency room. Bring your medication bottle with you.
Are there alternatives to macrolide antibiotics?
Yes. For many common infections - like strep throat, sinus infections, or bronchitis - antibiotics like amoxicillin, doxycycline, cephalexin, or levofloxacin are just as effective and carry no QT prolongation risk. Ask your doctor if a non-macrolide option is appropriate for your condition. Antibiotic stewardship isn’t just about resistance - it’s also about safety.



14 Comments
Curtis Younker January 25, 2026 AT 23:41
Man, I never thought about how a simple antibiotic could mess with your heart like that. I’ve had azithromycin for bronchitis three times and never even blinked. But now I’m sitting here Googling my own ECGs from last year. If you’re over 50, on any meds, or just feel kinda off after starting these pills - stop and ask. Seriously. Your heart doesn’t text you a warning. It just stops. And then it’s too late.
Shawn Raja January 26, 2026 AT 11:47
So let me get this straight - we’re telling people to avoid a $10 antibiotic because it might kill them… but we’ll still prescribe opioids for back pain that kills 70,000 a year? Classic American healthcare: prioritize the drama over the dead. The real tragedy isn’t QT prolongation - it’s that we treat patients like lab rats until something goes boom. Then we slap a black box on it and move on. #FirstWorldProblems
Ryan W January 27, 2026 AT 02:42
Incorrect. The FDA does NOT require a black box warning on clarithromycin for QT prolongation alone. The black box is for drug interactions via CYP3A4 inhibition - specifically with statins leading to rhabdomyolysis. You’re conflating two distinct mechanisms. Also, azithromycin’s 2.85x risk increase is relative risk, not absolute. Baseline CV mortality is 0.1% - so 0.285% is still statistically negligible for healthy patients. Don’t fearmonger with p-values.
Allie Lehto January 27, 2026 AT 03:38
OMG I JUST REALIZED MY DAD TOOK AZITHROMYCIN BEFORE HE HAD HIS HEART ATTACK 😭 I FEEL SO GUILTY I DIDN’T KNOW THIS. I’M GOING TO SEND THIS TO EVERYONE I KNOW. WE NEED TO MAKE THIS VIRAL. 🙏❤️ #HeartAwareness #DontLetThemDieLikeMyDad
Henry Jenkins January 28, 2026 AT 09:57
This is actually one of the most balanced and well-researched pieces I’ve read on antibiotic safety in years. I work in primary care and see macrolides prescribed like candy - especially for viral infections. The real issue isn’t just the drugs, it’s the culture of ‘quick fix’ medicine. Patients demand antibiotics. Doctors give them because it’s faster than explaining why they’re unnecessary. We need better tools - like that MARC calculator - and better education. Not just for patients, but for providers who think ‘it’s probably fine’.
Dan Nichols January 29, 2026 AT 19:18
QT prolongation? Sounds like another scare tactic from Big Pharma to sell ECG machines. If you’re healthy, don’t worry. If you’re not, you’re already on 12 other meds that are way worse. Stop listening to fear porn. Antibiotics save lives. Don’t let some 2012 study make you paranoid. Also, ECGs before every cold? Are you kidding me? We’re bankrupting the system with unnecessary testing.
Renia Pyles January 31, 2026 AT 01:24
So you’re telling me I can’t even take a Z-Pack without risking death? And my doctor didn’t even ask if I was on birth control? Or if I had a family history? I’m so mad right now. I’ve been taking azithromycin for years. My mom died at 52 from ‘sudden cardiac arrest’ - they never connected it. Now I’m terrified to even swallow a pill. Thanks for making me feel like my body is a ticking bomb.
Rakesh Kakkad February 1, 2026 AT 23:15
Dear American colleagues, in India, we rarely prescribe macrolides for upper respiratory infections due to widespread resistance. We use amoxicillin-clavulanate or doxycycline as first-line. Also, ECG screening is not feasible in rural clinics. Perhaps focus on rational prescribing rather than technological solutions. The root problem is antimicrobial misuse, not QT intervals.
Nicholas Miter February 3, 2026 AT 09:26
Had a friend go into TdP after a Z-Pack. She was 42, fit, no meds - but had low magnesium from drinking too much coffee and not eating. Weird, right? Point is, it’s not always the drug. It’s the combo. Maybe we need to stop thinking of antibiotics as isolated villains and start looking at the whole picture - diet, sleep, stress, other meds. It’s all connected. Just saying.
Suresh Kumar Govindan February 5, 2026 AT 03:07
Genetic screening before antibiotics? This is the beginning of medical totalitarianism. The state will soon require DNA tests for every prescription. Who will own your genome? The NIH? The FDA? The pharmaceutical lobby? This is not science - it is control. We are becoming data points, not patients.
TONY ADAMS February 6, 2026 AT 17:22
Bro I took azithromycin last week and felt weird but thought it was just the stomach stuff. Now I’m scared to even breathe. Should I go to the ER? I don’t wanna die.
George Rahn February 7, 2026 AT 12:26
They say azithromycin is ‘safer’ - but let’s be real. It’s still a chemical weapon disguised as medicine. We’ve turned our bodies into battlegrounds for profit-driven pharmacology. We’ve forgotten that nature gave us garlic, honey, and rest - not 12 different antibiotics for every sniffle. This isn’t progress. It’s surrender.
Ashley Karanja February 9, 2026 AT 00:57
As someone who’s worked in cardiac telemetry for 12 years, I’ve seen TdP up close - and it’s terrifying. One minute the patient’s stable, next they’re seizing on the monitor. The worst part? It’s often silent. No chest pain, no warning. Just a flatline. I wish every ER doc had that MARC calculator. I’ve watched too many patients get macrolides without a single check. If you’re over 60, female, on diuretics, or have any heart history - please, ask for an ECG. It takes 5 minutes. It could save your life.
Karen Droege February 9, 2026 AT 20:45
My sister’s cardiologist just told her to avoid all macrolides after she had a borderline QTc of 465. She’s 58, on a beta-blocker, and has mild mitral valve prolapse. She cried because she’s allergic to penicillin. So now what? She gets a 10-day course of doxycycline - which causes sunburns and GI hell. There’s no perfect option. We need better drugs, not just more warnings. And we need to stop acting like every patient is a liability. We’re all just trying to get better.