SSRI Risk Comparison Tool
This tool helps you understand the risk of hyponatremia (low sodium) from different antidepressants. Based on your age, gender, and health factors, it shows which medications carry lower risk for older adults.
Your Risk Profile
Answer these questions to see your risk level.
Why Your Antidepressant Might Be Lowering Your Sodium
Imagine waking up feeling off-not sick enough to call a doctor, but not right either. Headache. Nausea. A little confused. You think it’s just aging, or maybe the flu. But if you started an SSRI antidepressant two weeks ago, this could be something far more serious: hyponatremia. It’s not rare. It’s not theoretical. It’s happening to thousands of older adults right now, often unnoticed until it’s too late.
Hyponatremia means your blood sodium is too low-below 135 mmol/L. Sodium isn’t just table salt. It’s what keeps your nerves and muscles working, your brain functioning properly. When it drops too far, your cells swell. Your brain swells. That’s when confusion turns to seizures, coma, or death. And SSRIs? They’re one of the most common triggers.
How SSRIs Cause Low Sodium
SSRIs like sertraline, citalopram, and fluoxetine work by boosting serotonin in your brain. That’s how they help depression. But serotonin doesn’t just affect mood. It also talks to your hypothalamus-the part of your brain that controls water balance. When serotonin levels rise too much, your body releases too much antidiuretic hormone (ADH). That hormone tells your kidneys to hold onto water instead of peeing it out.
Result? You’re drinking the same amount of water, but your body is keeping more of it. Your blood gets diluted. Sodium levels drop. This isn’t dehydration-it’s the opposite. You’re waterlogged, not dry. And your sodium? It’s swimming in too much fluid.
This isn’t guesswork. Studies show a direct link between how strongly an SSRI binds to serotonin transporters and how likely it is to cause hyponatremia. Citalopram? Highest binding. Highest risk. Sertraline? Close behind. Fluoxetine? Still risky. Even paroxetine, often seen as "gentler," carries a real danger.
Who’s Most at Risk?
This isn’t a problem for everyone. But if you’re over 65, you’re in the danger zone. About 1 in 6 older adults starting an SSRI will develop low sodium. Women are more likely than men. People under 60 kg? Higher risk. Anyone on diuretics-especially thiazides like hydrochlorothiazide? Risk jumps 4 times. Kidney trouble? Even worse.
Here’s the scary part: many doctors don’t test for it. A 2023 survey found that over 60% of primary care doctors didn’t know hyponatremia from SSRIs usually shows up between 2 and 4 weeks after starting the drug. Patients? Only 29% were warned about it before taking the pill.
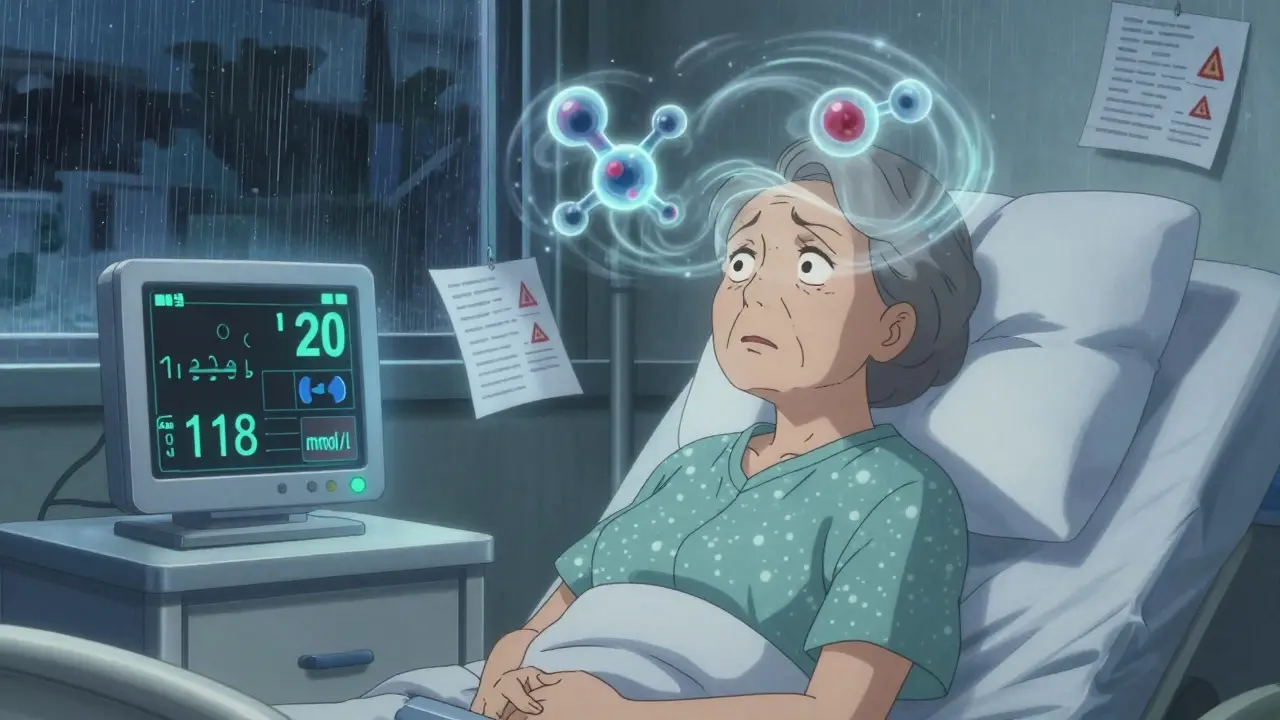
And because symptoms-headache, nausea, dizziness, confusion-look like dementia or just "getting older," they’re often ignored. A 78-year-old woman in a case report was admitted to the ICU after her sodium dropped to 118 mmol/L. She’d been on sertraline for 10 days. Her family thought she was just "acting strange." No one checked her blood.
What the Numbers Don’t Tell You
Let’s talk real numbers. For every 1,000 people taking an SSRI, about 19 will develop hyponatremia. That’s not a tiny risk. That’s like 1 in 50. For someone over 65? It’s closer to 1 in 7. Compare that to mirtazapine, another antidepressant: only 6-7 out of 1,000 develop low sodium. That’s a 3 times lower risk.
And here’s what no one talks about: cost. In the U.S. alone, SSRI-induced hyponatremia costs $1.27 billion a year. Most of that is hospital stays and ER visits. Think about that. Billions spent because a simple blood test could have prevented it.
And the FDA now requires all SSRI labels to include hyponatremia warnings. That’s not a small thing. It means regulators agree: this is a serious, documented danger.
What You Should Do Before Starting an SSRI
If you or a loved one is being prescribed an SSRI, here’s what you need to do-right now:
- Ask for a baseline blood test for sodium before starting the medication.
- Request a repeat test exactly two weeks after starting-or after any dose increase.
- Ask: "Is mirtazapine or bupropion an option?" Both have much lower hyponatremia risk.
- If you’re over 65, on diuretics, or have kidney issues, insist on monthly sodium checks for the first 3 months.
The American Psychiatric Association and the American Geriatrics Society both say this is standard care. If your doctor says it’s "not necessary," push back. This isn’t bureaucracy-it’s survival.
What If You Already Have Symptoms?
Confusion, nausea, headache, fatigue, muscle cramps-these are early red flags. If you’re on an SSRI and notice them, don’t wait. Get your sodium checked. Now.
If your sodium is below 135, the first step is stopping the SSRI. For mild cases (125-134 mmol/L), fluid restriction to 800-1,000 mL per day often fixes it within 72 hours. No drugs needed. Just water control.
But if sodium drops below 125? That’s an emergency. Hospital. IV fluids. Slow correction. Too fast, and you risk osmotic demyelination-a brain injury that can leave you locked in, unable to speak or move. Doctors have to correct sodium no faster than 6-8 mmol/L in 24 hours. That’s why timing matters.
Alternatives That Are Safer
You don’t have to risk your sodium to treat depression. Here’s what works better for older adults:
- Mirtazapine: Lowest risk. Helps with sleep and appetite too. Often preferred for elderly patients with weight loss or insomnia.
- Bupropion: Doesn’t affect serotonin much. Lower hyponatremia risk. Good if you need energy boost.
- Nortriptyline: A tricyclic with lower risk than amitriptyline. Still needs monitoring, but safer than SSRIs.
SSRIs still have their place-for younger people without other health issues. But for someone over 65? The data is clear: mirtazapine is the smarter first choice.

Why This Is Still Overlooked
Doctors aren’t ignoring this on purpose. They’re overwhelmed. Depression is common. SSRIs are easy to prescribe. Blood tests take time. Patients don’t report vague symptoms. And the benefits of treating depression are real-suicide risk drops, quality of life improves.
But here’s the truth: untreated depression kills. So does hyponatremia. The goal isn’t to avoid SSRIs entirely. It’s to avoid them blindly.
When a 82-year-old woman becomes confused after starting citalopram, and her sodium is 122, the problem isn’t the depression. It’s the lack of testing. The lack of awareness. The assumption that "it’s just aging." That’s what needs to change.
What’s Changing Now
Good news: things are shifting. Between 2018 and 2023, SSRI prescriptions for people over 65 dropped 22%. Mirtazapine prescriptions for the same group rose 35%. That’s not coincidence. That’s doctors learning.
The European Medicines Agency is reviewing SSRI safety. The first clinical algorithm for managing this exact problem was published in March 2024. And by 2027, mirtazapine is expected to be the top antidepressant for seniors.
This isn’t a future warning. It’s happening now. And the people who survive hyponatremia? Many are left with lasting brain fog, balance problems, or memory loss. Recovery takes weeks. Sometimes months.
Bottom Line: Don’t Guess. Test.
If you’re considering an SSRI-or already taking one-don’t assume it’s safe just because it’s common. Ask for a sodium test before you start. Ask for a repeat test two weeks later. Ask about safer alternatives. If you’re over 65, have kidney issues, or take water pills? This isn’t optional. It’s critical.
Depression matters. But so does your brain. And your sodium. One simple blood test can prevent a lifetime of consequences.
Can SSRIs cause confusion in older adults?
Yes. SSRIs can cause confusion in older adults by triggering hyponatremia-low sodium in the blood. When sodium drops below 135 mmol/L, brain cells swell, leading to disorientation, memory problems, and dizziness. These symptoms are often mistaken for dementia or aging, but they’re reversible if caught early with a blood test and stopping the SSRI.
How long after starting an SSRI does hyponatremia happen?
Hyponatremia usually develops between 2 and 4 weeks after starting an SSRI or increasing the dose. This is why doctors recommend a sodium blood test at the 2-week mark. Waiting longer risks missing the warning signs before they turn severe.
Which SSRI has the highest risk of causing low sodium?
Citalopram carries the highest risk, with studies showing a 2.37 times greater chance of causing hyponatremia compared to non-SSRI antidepressants. Sertraline and fluoxetine are also high-risk. Paroxetine and escitalopram carry moderate risk. The risk is linked to how strongly the drug binds to serotonin transporters in the brain.
Is mirtazapine safer than SSRIs for seniors?
Yes. Mirtazapine has a 3 times lower risk of causing hyponatremia than SSRIs. It doesn’t significantly affect serotonin in the same way, so it doesn’t trigger the hormone that causes water retention. For patients over 65, especially those with kidney issues or on diuretics, mirtazapine is now recommended as a first-line alternative by major psychiatric guidelines.
Should I get a blood test before starting an SSRI?
Absolutely. The American Psychiatric Association and American Geriatrics Society both recommend a baseline sodium test before starting any SSRI, especially for patients over 65, women, or those on diuretics. A second test at 2 weeks is critical. Many cases of hyponatremia are caught only after hospitalization-this is preventable.
Can hyponatremia from SSRIs be reversed?
Yes, if caught early. Stopping the SSRI and limiting fluid intake often restores sodium to normal within 3-4 days. In severe cases (below 125 mmol/L), hospitalization and slow IV correction are needed. But if correction is too fast, it can cause permanent brain damage. Timing and careful monitoring are everything.
Why don’t more doctors test for this?
Many primary care doctors aren’t trained to recognize this risk. A 2023 survey found that 63% didn’t know hyponatremia typically appears 2-4 weeks after starting an SSRI. Symptoms are vague and easily blamed on aging. But the data is clear: testing saves lives. It’s not extra-it’s standard care for high-risk patients.


14 Comments
Alex Warden January 2, 2026 AT 05:25
This is why America's healthcare is broken. Doctors prescribe SSRIs like candy and never check sodium. I'm a nurse in Chicago and I've seen 3 elderly patients end up in ICU over this. No one tests. No one cares. Just sign the script and move on. We're treating depression like it's a cold.
And don't even get me started on how Pharma pushes these drugs. They don't want you to know about mirtazapine. It's cheaper. It's safer. And it doesn't make them billions.
LIZETH DE PACHECO January 3, 2026 AT 16:49
Thank you for writing this. My mom started sertraline last month and suddenly she was forgetting her own phone number. We thought it was dementia. Turns out her sodium was 128. They admitted her, stopped the med, and she's back to herself in 5 days. This needs to be common knowledge. Not just for seniors-anyone on these meds should get tested.
Layla Anna January 3, 2026 AT 17:31
I'm so glad someone finally said this 😭 my grandma was on citalopram and kept saying she felt "foggy" but the doctor just told her to drink more water... turns out she was waterlogged not dehydrated. We caught it just in time but I still get nightmares thinking about what could've happened. Please please please ask for a blood test before starting any SSRI
jaspreet sandhu January 4, 2026 AT 11:27
You people act like SSRIs are some kind of poison. I've been on sertraline for 8 years. My sodium is fine. My brain is fine. My life is fine. You're scaring people with numbers and scare tactics. Depression is real. Not every old person needs to be treated like a lab rat. If you're healthy and your doctor says it's okay, stop freaking out. Not everyone is a walking electrolyte imbalance.
Heather Josey January 5, 2026 AT 06:45
I appreciate the thoroughness of this post. As a geriatric care coordinator, I can confirm that hyponatremia from SSRIs is underdiagnosed and often misattributed to cognitive decline. The recommendation for baseline and 2-week sodium testing aligns with current clinical guidelines. I encourage all clinicians to adopt this as routine practice, particularly for patients on diuretics or with renal impairment. Prevention is not optional-it is standard of care.
Donna Peplinskie January 5, 2026 AT 20:45
I just want to say... thank you. I'm so tired of people saying "oh it's just aging" when someone starts acting confused. My aunt was like that-quiet, withdrawn, forgetful. We thought it was Alzheimer's. Turned out it was sertraline. She's fine now. But she lost three months of her life to this. Please, if you're caring for someone older, just ask for the blood test. It takes five minutes. It could save their brain.
Olukayode Oguntulu January 6, 2026 AT 02:37
Ah yes, the neoliberal pharmacological colonization of the elderly psyche. SSRIs as biopolitical tools of social control-pathologizing normal affective fluctuations under the guise of mental health. The FDA warning? Merely performative. Capitalism commodifies distress and then monetizes its iatrogenic consequences. The real crisis isn't hyponatremia-it's the epistemic violence of biomedical hegemony. Mirtazapine? A palliative for the hegemonic regime. We must deconstruct the serotonin mythos entirely.
Bryan Anderson January 7, 2026 AT 16:59
I work in a rural clinic and this is exactly what we're seeing. Patients come in with confusion, we run labs, sodium is low, they're on an SSRI. We switch them to mirtazapine and they’re like a different person in two weeks. The problem isn't the medication-it's the lack of follow-up. Most of our patients don’t even have primary care. They get the script, take it, and vanish. Testing isn’t happening. We need systems-not just awareness.
Matthew Hekmatniaz January 8, 2026 AT 12:45
I'm an immigrant from Mexico and my dad started fluoxetine last year. He got really confused, started mixing up names, didn't recognize me. We thought it was the stroke he had last year. Turns out, it was the pill. We got his sodium checked and it was 129. They stopped it, gave him fluids, and he came back. I didn't know any of this. No one told us. This needs to be translated into Spanish. Into Tagalog. Into Arabic. This isn't just an American problem.
Liam George January 9, 2026 AT 20:59
This is all a distraction. The real issue? The government is using SSRIs to chemically suppress the elderly population so they don't vote. Low sodium = brain fog = less likely to question the system. The FDA warning? A smokescreen. The same people who pushed these drugs are the ones writing the guidelines. They're making billions. And now they want you to think testing is the solution. It's not. It's just another control mechanism. Don't take the pill. Don't trust the test. Trust nothing.
sharad vyas January 10, 2026 AT 14:23
I've been thinking about this a lot. We treat depression like it's a broken gear that needs replacing. But maybe the whole machine is wrong. Why do we assume every old person who feels sad needs a chemical fix? What if we tried community, quiet walks, family meals, sunlight? Maybe the real cure isn't in the pill but in the way we've stopped being human to each other. The sodium test is good. But we need more than tests. We need more presence.
Paul Ong January 11, 2026 AT 14:33
My uncle died from this. No one knew. He was on citalopram. Confused. Then coma. Then gone. Don't wait. Test. Now. Seriously.
Andy Heinlein January 11, 2026 AT 15:54
Just had this happen with my neighbor. She was on sertraline, got dizzy, fell, broke her hip. Turns out her sodium was 126. She's 84. They switched her to mirtazapine and she's baking cookies again. This is wild. We need to talk about this more. Like, everywhere.
Todd Nickel January 12, 2026 AT 00:23
The data presented here is methodologically sound. The 19 per 1,000 incidence rate for hyponatremia among SSRI users is corroborated by multiple cohort studies including the 2022 JAMA Psychiatry meta-analysis. The differential risk profile among SSRIs-citalopram > sertraline > fluoxetine > paroxetine-is consistent with receptor binding affinity metrics (Ki values for SERT). The recommendation for sodium monitoring at 2 weeks aligns with the pharmacokinetic half-life of most SSRIs and the typical onset window for SIADH. The assertion that mirtazapine presents a lower risk is supported by its minimal effect on serotonin reuptake and lack of ADH stimulation. This is not anecdotal. It is evidence-based medicine. The failure to implement routine screening is a systemic failure of clinical protocol adherence, not a lack of evidence.