When your big toe suddenly swells up, turns red, and feels like it’s on fire-especially at night-you’re not just having a bad night. You’re likely experiencing a gout flare. This isn’t just pain from overdoing it at the bar or eating too much steak. It’s a direct result of how your body breaks down purines, and whether or not your kidneys can keep up. Gout affects nearly 8.3 million Americans, and for many, it’s not a one-time event. It’s a lifelong condition that needs real, science-backed management.
What Exactly Is Happening in Your Body?
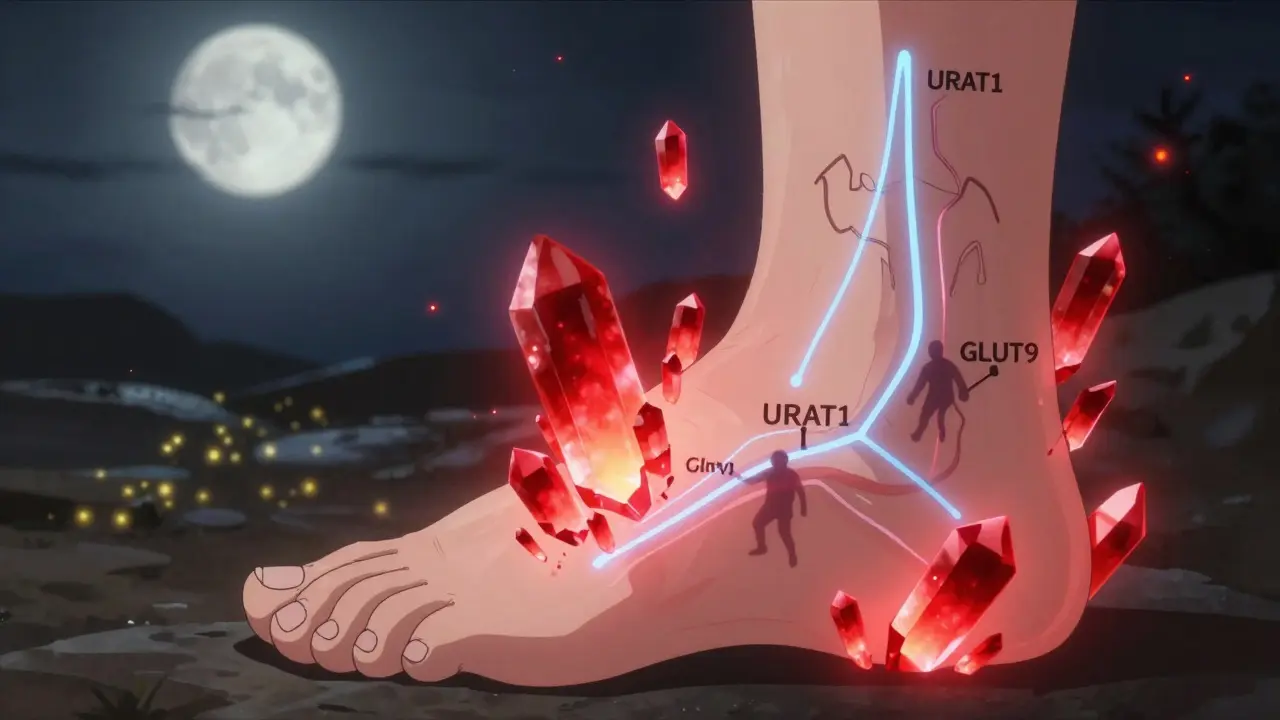
Your body breaks down purines-natural compounds found in your cells and in certain foods-into uric acid. Normally, that uric acid dissolves in your blood, gets filtered by your kidneys, and leaves your body through urine. But when too much is made or your kidneys can’t remove it fast enough, uric acid builds up. At levels above 6.8 mg/dL, it starts forming sharp, needle-like crystals in your joints. That’s gout. This isn’t new. Hippocrates wrote about it over 2,000 years ago, calling it the "disease of kings" because it often showed up in people who ate rich foods and drank too much wine. But the real culprit isn’t just diet. It’s biology. Humans lost the enzyme uricase about 15-20 million years ago. That enzyme, which breaks down uric acid into something harmless, is still active in most animals. We don’t have it. So we’re stuck with uric acid as the final waste product. About 65% of uric acid leaves through your kidneys. But here’s the twist: 90% of what your kidneys filter gets reabsorbed back into your blood. That’s because of transporters like URAT1 and GLUT9. These proteins act like bouncers, letting uric acid back in. If they’re overactive-or if your body makes too much uric acid to begin with-you’re at risk.How Purine Metabolism Goes Off the Rails
Purines come from two places: your own cells (80%) and what you eat (20%). When your cells die, they release nucleotides. These get broken down step by step: first into nucleosides, then into bases like hypoxanthine and guanine, then into xanthine, and finally into uric acid. The last step is handled by an enzyme called xanthine oxidase. If something goes wrong in this chain-like a rare genetic defect in HPRT (hypoxanthine-guanine phosphoribosyltransferase)-you make way too much uric acid. That’s Lesch-Nyhan syndrome, a severe condition seen in children. But even without a genetic flaw, your body can overproduce uric acid if you have high levels of PRPP (phosphoribosyl pyrophosphate), which speeds up purine production. Alcohol, especially beer, boosts PRPP. So does obesity and insulin resistance. On the flip side, if your kidneys aren’t working well, uric acid piles up even if your body isn’t overproducing it. That’s why gout is so common in people with chronic kidney disease. And it’s why some people can eat a clean diet and still get gout-their kidneys just can’t keep up.Urate-Lowering Medications: The Three Main Types
The goal of treatment isn’t just to stop a flare. It’s to lower your serum uric acid level below 6.0 mg/dL-sometimes even below 5.0 mg/dL if you have tophi (those visible lumps of uric acid crystals under the skin). That’s the only way to dissolve existing crystals and prevent new ones. There are three classes of drugs that do this, each with a different strategy:- Xanthine oxidase inhibitors (XOIs): Block the final step of uric acid production.
- Uricosurics: Help your kidneys flush out more uric acid.
- Uricase agents: Turn uric acid into a soluble compound your body can easily remove.
Allopurinol and Febuxostat: The First-Line Choices
Allopurinol is the oldest and cheapest option. It’s been around since 1966. Generic versions cost about $4.27 a month. It works by blocking xanthine oxidase, the enzyme that turns xanthine into uric acid. But here’s the catch: most people don’t take enough. Studies show 92% of patients hit their target uric acid level only when allopurinol is increased to 300 mg or more per day. Yet many doctors start at 100 mg and never adjust. That’s why so many people think it doesn’t work. Febuxostat, approved in 2009, is stronger. At 80 mg a day, it gets 66.7% of patients to target levels, compared to 46.7% with allopurinol. But it’s expensive-around $59 a month-and carries a black box warning from the FDA. A major 2018 trial found it increased the risk of heart-related death in people with existing heart disease. So if you have heart problems, allopurinol is still the safer bet.Probenecid and Lesinurad: Helping Kidneys Do Their Job
Probenecid has been used since 1949. It blocks URAT1, the transporter that pulls uric acid back into your blood. That means more uric acid gets flushed out. But it only works if your kidneys are still functioning well-creatinine clearance must be above 50 mL/min. It’s also not great for people with kidney stones, since it increases uric acid in the urine. Lesinurad was approved in 2015 and was meant to be used with allopurinol. It boosted success rates to 54%. But it was pulled from the market in 2019 because of serious kidney damage. So it’s no longer available in the U.S.Pegloticase: The Nuclear Option
Pegloticase is a biologic drug. It’s an engineered version of uricase-the enzyme humans lost. It breaks down uric acid into allantoin, which is easily excreted. It’s powerful: 42% of patients hit target levels within six months. For those with severe tophaceous gout, it can make tophi disappear. But it’s not simple. It’s given by IV every two weeks. It costs over $16,000 a month. And 26% of patients have infusion reactions-rash, chest pain, even anaphylaxis. You need to be pre-medicated and monitored. Plus, your body can develop antibodies against it, making it stop working. Only a handful of rheumatologists use it, and insurers make you jump through hoops just to approve it. One patient on Reddit said they needed 17 prior authorizations.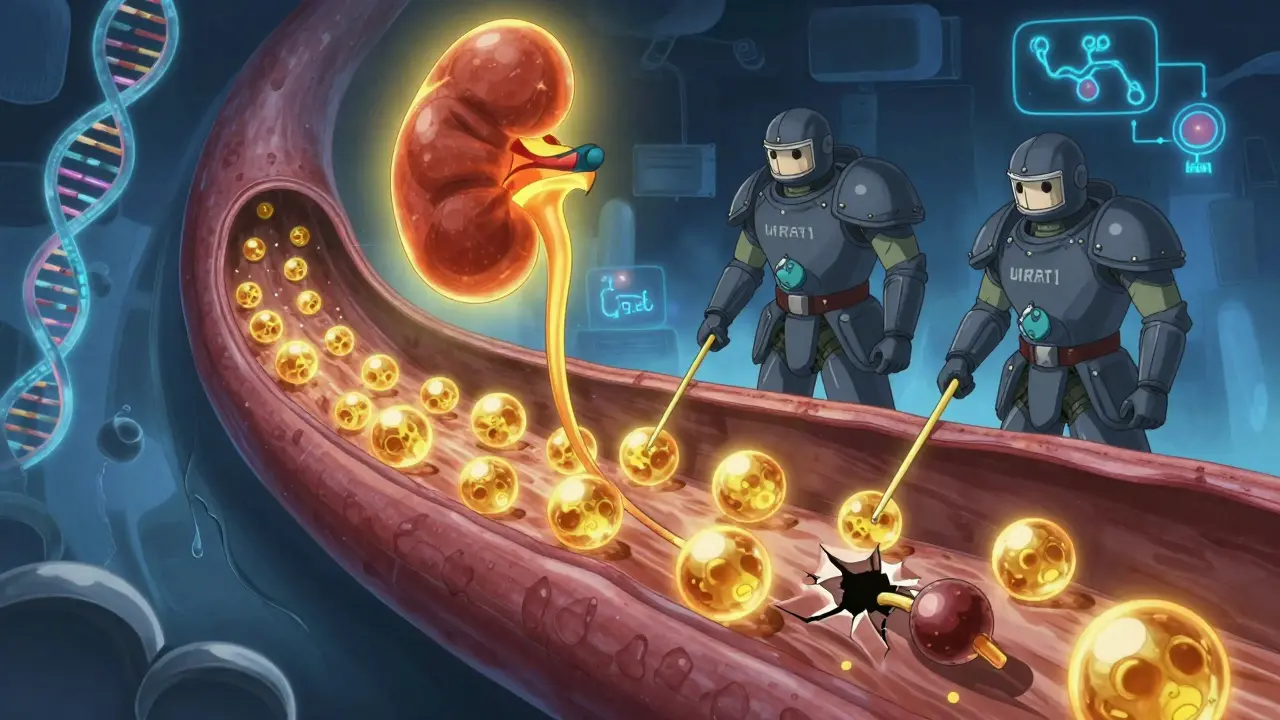
Why So Many People Stop Taking Their Medication
The real problem isn’t that these drugs don’t work. It’s that people stop taking them. A 2022 survey found 61% of gout patients quit their urate-lowering therapy within a year. Why? Three main reasons:- 33% thought it wasn’t working-but they didn’t realize it takes months to dissolve crystals.
- 29% had side effects-rash with allopurinol, liver issues with febuxostat.
- 18% found the dosing too complicated-especially when they’re told to take colchicine too.
Diet Matters-But Not Like You Think
You’ve probably heard to avoid red meat, shellfish, and beer. That’s true. Organ meats like liver have 240-400 mg of purines per 100 grams. Anchovies? 500 mg. Beer? 10-20 grams of purines per liter. But here’s the truth: diet alone rarely drops your uric acid by more than 1-2 mg/dL. That’s not enough to get you below 6.0 mg/dL if you’re at 9.0. So while cutting back on beer and steak helps, it won’t fix the problem alone. What’s more surprising? Sugar-especially fructose-is a big driver. Soda, sweetened juices, and processed foods spike uric acid. That’s why gout is rising alongside obesity and metabolic syndrome. In fact, 65% of gout patients have high blood pressure. It’s not just about what you eat. It’s about how your body handles sugar and fat.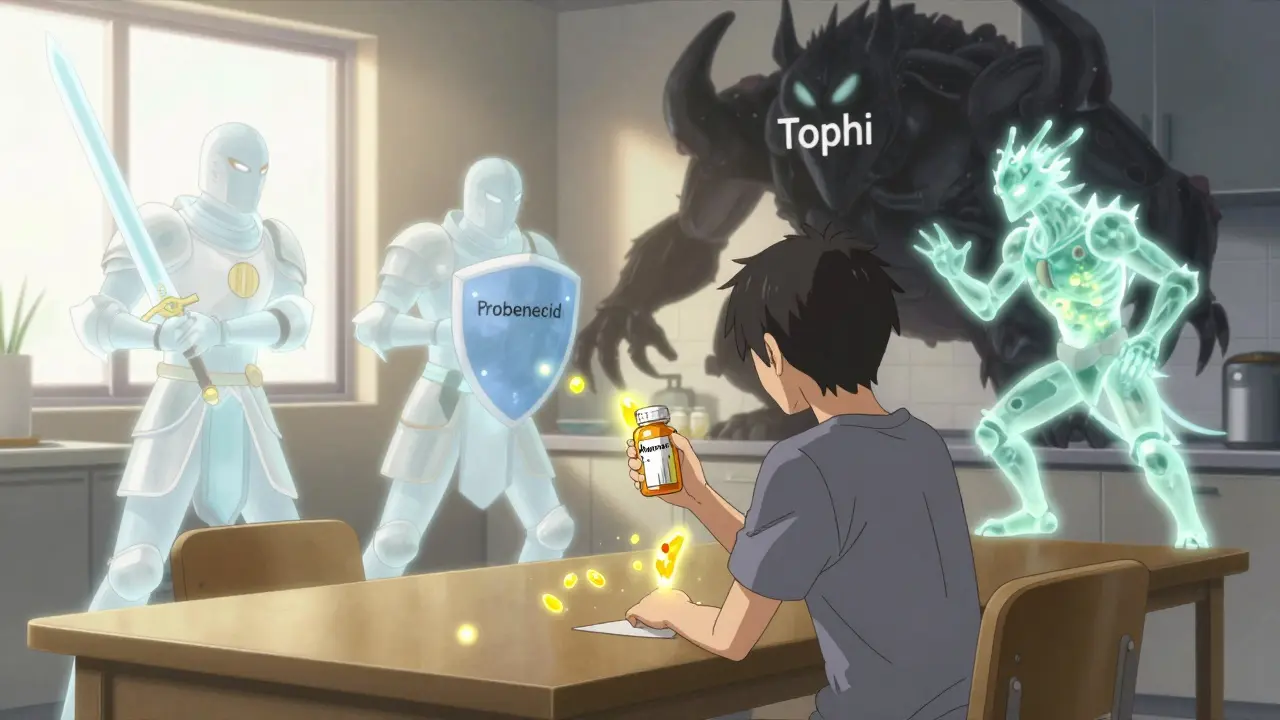
The Future of Gout Treatment
New drugs are on the horizon. Verinurad, a selective URAT1 blocker, is in Phase III trials. When combined with febuxostat, it got 74% of patients to target levels in just 12 weeks. That’s promising. Arhalofenate is another one. It doesn’t just lower uric acid-it also reduces inflammation. In a 2024 trial, it cut flare frequency by 58% compared to placebo. And there’s growing interest in personalized medicine. Some people have genetic variants in SLC2A9, a gene that controls how your kidneys handle uric acid. If you have a certain version, you might respond better to uricosurics. In the future, a simple genetic test could tell you which drug to start with. But until then, the best approach is still simple: start low, go slow, monitor your uric acid every 2-5 weeks until you hit target, and never stop your medication just because you feel fine. Gout isn’t cured by one flare-free month. It’s managed by years of steady, low uric acid levels.What You Can Do Right Now
- If you’re on allopurinol and still having flares, ask your doctor if your dose is high enough. 300 mg is often the minimum effective dose.
- If you’re on febuxostat and have heart disease, talk to your doctor about switching to allopurinol.
- Ask for a serum uric acid test every 6 months-even if you feel fine.
- Don’t skip colchicine if you’re starting ULT. It’s not a side effect-it’s part of the plan.
- Limit sugary drinks and beer. Swap them for water and coffee. Both are linked to lower gout risk.
Can gout be cured with diet alone?
No. While avoiding high-purine foods like organ meats and beer can help, diet alone typically lowers uric acid by only 1-2 mg/dL. Most people need medication to reach the target level of 6.0 mg/dL or lower. Diet is a support tool, not a cure.
Why do I have more gout flares after starting allopurinol?
That’s normal. When uric acid crystals start to dissolve, they trigger inflammation. This doesn’t mean the drug isn’t working-it means it is. Doctors recommend taking colchicine for at least six months when starting urate-lowering therapy to prevent these flares.
Is febuxostat safer than allopurinol?
Not for everyone. Febuxostat is more effective at lowering uric acid, but it carries a black box warning for increased risk of heart-related death, especially in people with existing heart disease. Allopurinol is safer for most patients and is still the first-line recommendation.
How often should I get my uric acid level checked?
When starting or adjusting medication, check every 2-5 weeks until you hit your target (under 6.0 mg/dL). Once stable, check every 6 months. Many doctors don’t follow this, but it’s critical-uric acid levels can creep up without symptoms.
What’s the cheapest effective treatment for gout?
Generic allopurinol is the most cost-effective option, costing as little as $4.27 per month. It’s effective when taken at the right dose (usually 300 mg or higher). The key isn’t the drug-it’s making sure you’re on enough of it.
Can I stop taking my gout medication if I haven’t had a flare in a year?
No. Gout is a chronic condition. Stopping medication allows uric acid to rise again, and crystals will reform. Even if you haven’t had a flare in years, stopping treatment puts you at risk for joint damage, tophi, and kidney problems. Lifelong therapy is the standard.


11 Comments
dean du plessis December 27, 2025 AT 18:10
Interesting breakdown. I’ve seen this play out in my uncle’s life-he’s had gout for 15 years, never missed a dose of allopurinol, and still drinks his daily soda. The real villain isn’t the steak, it’s the high-fructose corn syrup in everything. His uric acid dropped 3 points after he switched to water and black coffee. No magic, just science.
Also, never heard that we lost uricase 20 million years ago. Makes you wonder how many other biological quirks we’re stuck with because evolution didn’t bother fixing them.
Anyway, thanks for the clarity.
Anna Weitz December 28, 2025 AT 14:46
So we’re all just broken primates with bad kidneys and a sweet tooth and somehow this is a disease of kings lmao
Caitlin Foster December 28, 2025 AT 18:42
OH MY GOD YES. I’ve been telling my doctor for YEARS that allopurinol wasn’t working-and he kept saying ‘it’s working, you just need to wait!’ Wait? I was in a wheelchair for three weeks. Then I asked for 300mg and BOOM-no flares in 11 months. Why do doctors treat gout like it’s a cold??
Also, colchicine is not optional-it’s your body’s tiny bodyguard. Take it. Please.
And stop drinking orange juice. It’s not ‘healthy.’ It’s liquid sugar with a vitamin C sticker.
Andrew Gurung December 29, 2025 AT 16:51
Of course you need to take colchicine. But let’s be real-most people don’t even know what uric acid is. They think gout is ‘a punishment for partying too hard.’ And yet, they’ll spend $80 on a bottle of ‘gout detox’ tea while ignoring their actual meds.
I’ve seen patients who’ve lost 40 pounds, quit alcohol, and still have tophi because they stopped their pills after six months. It’s not about willpower. It’s about understanding that gout is a metabolic disease, not a moral failing.
And if you think febuxostat is ‘better’ without checking your heart history-you’re not just uninformed, you’re dangerous.
Also, I’m not even mad about the $16,000/month pegloticase. I’m mad that it took 50 years for someone to finally bring back uricase. We lost it 20 million years ago and now we’re playing catch-up with biotech. Pathetic.
Alex Lopez December 29, 2025 AT 17:45
While I appreciate the clinical precision of this post, I must note that the underlying assumption-that patients are simply noncompliant-is a dangerous oversimplification. The healthcare system in this country is designed to make adherence nearly impossible: high drug costs, lack of follow-up, minimal patient education, and the normalization of chronic pain as ‘just part of aging.’
When a patient is told, ‘Take this pill every day for life, and if you stop, you’ll damage your joints,’ without being shown a diagram of uric acid crystals, without being given a printed schedule, without being offered a telehealth check-in, then yes, they will stop. Not because they’re lazy. Because they’re overwhelmed.
Also, the fact that lesinurad was pulled from the market due to renal toxicity, yet allopurinol (which causes life-threatening SJS in HLA-B*58:01 carriers) remains first-line without mandatory genetic screening… that’s not medicine. That’s roulette.
And for the record: yes, I’m a rheumatologist. And yes, I still have to fight insurance for pegloticase. The system is broken. The science? Brilliant. The delivery? Catastrophic.
Paula Alencar December 30, 2025 AT 13:09
Let me just say this with all the emotional weight of someone who has watched three family members lose their mobility to gout: this is not a lifestyle choice. It is not a punishment. It is not a ‘you ate too much shrimp’ situation. It is a biochemical cascade that has been misunderstood for centuries-and we are finally, FINALLY, beginning to understand it.
When you say ‘diet doesn’t matter,’ people hear ‘it’s not your fault.’ And that is the most powerful thing you can say to someone who has been shamed for decades. ‘Oh, you drink beer? No wonder you have gout.’ No. You have gout because your kidneys reabsorb too much uric acid, and your body lacks the enzyme to break it down, and your genes made you vulnerable.
So if you’re on medication and still having flares-don’t quit. Don’t feel guilty. Don’t think you’re failing. You’re not. You’re fighting a war your body was never meant to win. And you’re doing it with science. And that? That’s heroic.
Also-coffee. Drink coffee. It’s the only beverage that’s both a ritual and a treatment.
Gerald Tardif January 1, 2026 AT 01:48
My dad was on allopurinol for 12 years and never once got his uric acid checked. He thought if he didn’t feel pain, he was fine. Then he got a tophus on his elbow. Big, ugly, visible lump. He cried when he saw it. Said he didn’t know it could do that.
Now he checks his levels every 6 months. Takes colchicine. Swears by black coffee. And yes-he still eats steak. But now he knows it’s not the steak. It’s the silence.
Doctors need to talk more. Patients need to listen more. And we all need to stop pretending this is just ‘a bad toe.’ It’s a whole-body thing.
Good post. Thanks for saying what needs to be said.
Will Neitzer January 1, 2026 AT 16:20
There is a critical omission in this otherwise excellent exposition: the role of insulin resistance in uric acid retention. Hyperinsulinemia directly stimulates URAT1 and GLUT9 transporters in the proximal tubule, thereby increasing uric acid reabsorption. This is why metabolic syndrome and gout are so tightly linked-not merely coincidental, but mechanistically intertwined.
Furthermore, the suggestion that ‘diet alone rarely drops uric acid by more than 1–2 mg/dL’ is statistically accurate but clinically misleading. In patients with mild hyperuricemia and no renal impairment, dietary modification combined with weight loss can reduce serum urate by up to 3.5 mg/dL, particularly when fructose and alcohol are eliminated.
It is not that diet is insufficient-it is that it is often applied too late, too weakly, and without proper monitoring. The true failure lies not in the biology of gout, but in the failure of preventive medicine.
Finally, I would add that the emerging data on arhalofenate’s dual anti-inflammatory and urate-lowering effects may represent the first true disease-modifying agent for gout, not merely a symptomatic one. This deserves far more attention.
Chris Garcia January 2, 2026 AT 09:34
Back home in Nigeria, we don’t have gout clinics. We have grandmas who brew bitter leaf tea and say, ‘Your blood is thick.’ They’re not wrong. Uric acid is thick. It’s sticky. It’s like syrup in your joints.
But here’s the thing-our people don’t drink soda. We don’t eat processed food. We eat yam, plantain, okra, fish, and palm oil. And yet, gout is rising. Why? Because now we have sugar in our tea. Because now we drink beer to look ‘modern.’ Because now we sit all day and don’t walk to the market.
This isn’t just an American problem. It’s a global betrayal of our biology. We traded ancient rhythms for convenience. And now our bodies are revolting.
So yes, take your pills. But also, walk. Drink water. Stop the sugar. Don’t wait for a flare to start caring.
And if you’re a doctor reading this? Don’t just prescribe. Educate. In our language. In our context. Gout doesn’t care about your fancy journal. It cares if you taught someone how to live.
Monika Naumann January 4, 2026 AT 06:31
It is deeply concerning that this article casually dismisses the moral responsibility of dietary discipline. In many cultures, including my own, gluttony and indulgence are not merely personal choices-they are spiritual failures. The ancient Greeks understood this. The Bible speaks of drunkenness and excess. And yet, we now reduce a divine warning to a transporter protein.
Yes, genetics play a role. Yes, uricase was lost. But the human body was designed for moderation. When we ignore this, we invite suffering-not as a biological accident, but as a consequence of moral decay.
Allopurinol is not a license to eat lobster every night. It is a mercy, not a mandate.
Let us not mistake medical progress for moral relativism.
dean du plessis January 5, 2026 AT 02:21
Man, I just read your comment about moral decay and I had to laugh. So you’re saying if my uncle had just prayed harder, he wouldn’t have lost three toes to tophi? Or maybe he just didn’t love God enough?
Look, I get it. You want to believe this is about sin. But your grandma’s bitter leaf tea didn’t dissolve his crystals. Allopurinol did. And the fact that he’s still alive, still walking, still eating yams and fish without a flare? That’s not divine intervention. That’s science.
Let’s not turn medicine into a sermon. People are suffering. They need help, not judgment.