Black Box Warning Risk Assessment Tool
This tool helps you understand your potential risk level for serious side effects associated with medications that carry FDA black box warnings. It's not medical advice - always consult your healthcare provider.
Your Risk Assessment
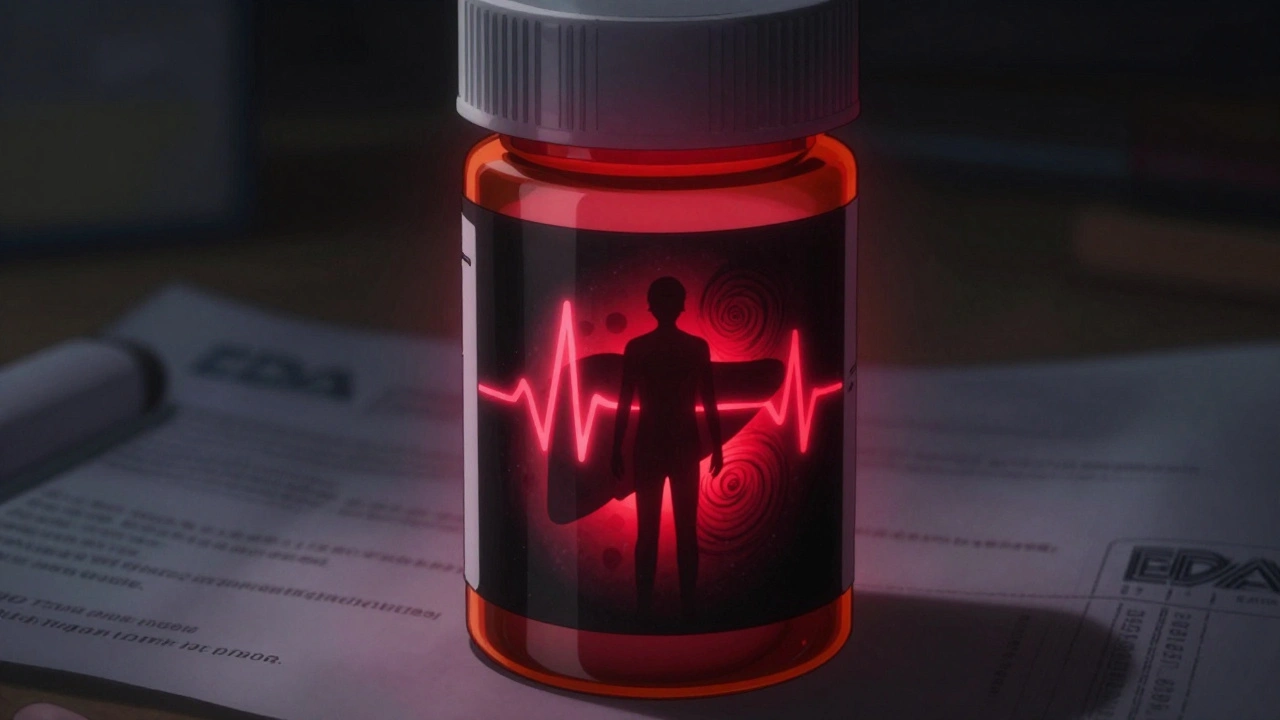
When you pick up a prescription, you might not notice the small black rectangle on the label. But that box? It’s the FDA’s loudest possible warning: this drug can kill you. More than 400 medications in the U.S. carry this warning - not as a suggestion, not as a footnote, but as a legally required alert stamped in bold black borders. These aren’t minor side effects like dizziness or dry mouth. These are risks that can lead to sudden death, organ failure, or irreversible harm. And yet, many patients never hear about them until they’re already taking the drug.
What Exactly Is a Black Box Warning?
A black box warning, officially called a boxed warning, is the highest safety alert the FDA can require for a prescription drug. It’s not optional. It’s not buried in fine print. It’s placed at the very top of the drug’s prescribing information, surrounded by a thick black border so doctors and pharmacists can’t miss it. The FDA mandates this format under 21 CFR 201.56 and 201.57 to make sure the most dangerous risks stand out.These warnings aren’t about inconvenience. They’re about life or death. They flag risks like:
- Sudden heart failure or fatal arrhythmias
- Severe liver damage
- Increased risk of suicide in young adults
- Life-threatening infections from immune system suppression
- Birth defects when taken during pregnancy
For example, the diabetes drug rosiglitazone (Avandia) got a black box warning in 2007 after studies linked it to a 43% higher risk of heart attack. The warning didn’t pull the drug off the market - it forced doctors to weigh the benefits against the risk for each patient. Some patients still take it, but only after a detailed discussion about alternatives.
How Does the FDA Decide to Add a Black Box Warning?
You might assume the FDA catches all serious risks before a drug hits the market. But that’s not how it works. Most black box warnings come after the drug is already being used by hundreds of thousands of people.The FDA relies on real-world data collected through the MedWatch program. Every year, about 1.3 million reports of side effects pour in - from doctors, pharmacists, patients, and drug companies. When a pattern emerges - say, five different reports of sudden liver failure in young women taking the same medication - the FDA investigates.
If the evidence shows the risk is serious enough to outweigh the benefit for some patients, the agency issues the warning. It’s not about perfection. It’s about recognizing danger when it becomes undeniable. The FDA doesn’t wait for a hundred deaths. Sometimes, a dozen confirmed cases are enough to trigger the warning.
Take the antidepressant fluoxetine (Prozac). In 2004, the FDA added a black box warning after data showed a doubled risk of suicidal thoughts in teens and young adults during the first few weeks of treatment. The warning didn’t stop the drug from being used - it changed how doctors monitor patients. Now, follow-up visits are required within the first month.
Why Do Some Drugs With Black Box Warnings Still Get Prescribed?
If a drug can kill you, why is it still on the shelf? The answer is simple: sometimes, the alternative is worse.Consider clozapine, a powerful antipsychotic used for treatment-resistant schizophrenia. It carries a black box warning for agranulocytosis - a condition where white blood cells drop to dangerously low levels, leaving the body defenseless against infection. About 1% of patients develop this. But for people who’ve tried every other antipsychotic and still hear voices or feel paranoid, clozapine can be the only thing that restores their life.
Doctors don’t ignore black box warnings. They use them as a checklist. Before prescribing, they ask:
- Is there a safer alternative?
- Does the patient have other conditions that make this risk worse?
- Can we monitor for early signs of trouble?
- Will the patient actually follow up for blood tests or check-ups?
For some patients, the benefit - like surviving a deadly cancer or managing a debilitating mental illness - outweighs the risk. The warning doesn’t say “don’t use.” It says, “use with extreme caution, and only if you understand what you’re risking.”
What Should You Do If Your Medication Has a Black Box Warning?
Don’t panic. Don’t stop cold turkey. Do this instead:- Ask your doctor to explain the warning in plain language. What exactly could go wrong? How often does it happen?
- Find out what monitoring is required. Do you need monthly blood tests? Liver scans? Heart checks? If your doctor doesn’t mention monitoring, ask.
- Ask about alternatives. Is there another drug with similar effectiveness but fewer risks? For example, instead of pioglitazone (which has a black box warning for bladder cancer), some doctors now prescribe GLP-1 agonists like semaglutide.
- Know the red flags. If you’re on a drug with a black box warning for liver damage, watch for yellow skin, dark urine, or constant nausea. For suicide risk, watch for sudden mood shifts or talking about hopelessness. Report these immediately.
- Report side effects. If you experience something bad, report it to MedWatch. The FDA needs real-world data to spot new dangers.
Many patients don’t realize they’re taking a drug with a black box warning. The warning isn’t on the pill bottle - it’s in the prescribing information. If you’re unsure, ask your pharmacist for the full drug facts sheet. Or look up your medication on the FDA’s Drugs@FDA database. It’s free, public, and updated daily.
Black Box Warnings Aren’t the Whole Story
A black box warning doesn’t mean a drug is dangerous for everyone. It means it’s dangerous for some people - and the FDA wants you to know who those people might be.Take the birth control pill Yaz. It carries a black box warning for blood clots. But the risk is highest in women over 35 who smoke. For a healthy 25-year-old non-smoker, the risk is extremely low. The warning doesn’t ban the drug - it tells doctors to screen for risk factors before prescribing.
Also, not all serious side effects get a black box warning. Some drugs have strong warnings about nausea or dizziness - important, but not life-threatening. The FDA reserves black box warnings for the worst-case scenarios. That’s why they’re so rare, and so powerful.

What Happens After a Black Box Warning Is Issued?
Once a warning is added, things change. Prescriptions often drop by 25% to 40% in the first year. But for drugs treating serious conditions, usage doesn’t vanish. Patients and doctors make hard choices.Take the cancer drug vemurafenib. After a black box warning for skin cancer risk, prescriptions fell - but not for patients with advanced melanoma who had no other options. The warning didn’t stop treatment. It changed how doctors monitored for new moles and skin lesions.
The FDA doesn’t leave warnings static. If new data shows the risk is lower than thought - or if better monitoring reduces harm - the warning can be updated. In 2020, the FDA revised the black box warning for the diabetes drug metformin after new evidence showed it was safer for kidney patients than previously believed.
And now, the FDA is moving toward smarter warnings. In its 2023-2027 plan, the agency says it wants to include genetic risk markers. For example, instead of saying “this drug can cause liver damage,” future warnings might say, “this drug can cause liver damage in patients with the HLA-B*57:01 gene variant.” That’s precision medicine in action.
Bottom Line: Don’t Fear the Box - Understand It
A black box warning isn’t a death sentence. It’s a conversation starter. It’s a signal that this drug has serious risks - but also serious benefits. The goal isn’t to scare you off. It’s to make sure you and your doctor make a decision based on facts, not guesswork.If you’re on a medication with a black box warning, you’re not alone. Millions of Americans are. But you’re also in a better position than most - because now you know to ask the right questions. Talk to your doctor. Get the facts. Know what to watch for. And never assume a warning means you can’t use the drug. It means you need to use it wisely.
Are black box warnings the same as recalls?
No. A recall means the drug is pulled from the market because it’s unsafe or defective. A black box warning means the drug stays on the market, but with strict safety alerts. The FDA doesn’t remove the drug - it adds a warning to help doctors and patients use it more safely.
Can I still take a drug with a black box warning if I’m healthy?
Yes - if your doctor believes the benefits outweigh the risks for you. Many people with serious conditions like epilepsy, depression, or autoimmune diseases take black box drugs safely because they have no better options. The key is monitoring and open communication with your provider.
Do over-the-counter drugs have black box warnings?
No. Black box warnings only apply to prescription drugs. Over-the-counter medications have different labeling rules. But that doesn’t mean OTC drugs are risk-free - acetaminophen, for example, can cause liver failure if taken in high doses.
How do I find out if my medication has a black box warning?
Check the FDA’s Drugs@FDA database. Search your drug by name, then click on the “Labeling” link. Look for the “Boxed Warning” section near the top. Your pharmacist can also give you the full prescribing information sheet. Don’t rely on the pill bottle - the warning isn’t printed there.
Can a black box warning be removed?
Yes. If new studies show the risk is lower than originally thought - or if monitoring protocols make the drug safer - the FDA can remove or revise the warning. For example, the warning for metformin was updated in 2020 after new data showed it was safe for patients with mild kidney issues.
If you’re taking a medication with a black box warning, your next step is simple: call your doctor or pharmacist. Ask them to walk you through the warning. Write down the risks, the monitoring plan, and the signs to watch for. Knowledge isn’t just power - it’s protection.


14 Comments
Kumar Shubhranshu December 5, 2025 AT 20:45
Black box warnings are just bureaucracy playing god. If you're dumb enough to not read the label, you deserve what you get. Simple as that.
Mayur Panchamia December 6, 2025 AT 22:36
Ohhhhh so NOW the FDA gives a damn?!? For decades they let Big Pharma poison us with ‘miracle drugs’ while sipping champagne in D.C.! They only act when the bodies pile up-like clockwork! This isn’t safety-it’s damage control with a fancy border!
Nava Jothy December 6, 2025 AT 23:00
I can't believe people still trust Big Pharma... 🙄 I had a friend on Avandia-she had a heart attack at 38. The doctor said ‘it’s rare’-but ‘rare’ doesn’t mean ‘won’t happen to you.’ I cried for weeks. And now? They just slap a black box on it like it’s a coupon for caution. 😔
brenda olvera December 8, 2025 AT 16:31
My grandma takes clozapine and she’s been stable for 8 years. She laughs again. She eats with her hands. That’s worth the risk. We check her blood every week. That’s not fear-that’s love.
Myles White December 8, 2025 AT 17:14
It's fascinating how the FDA's post-market surveillance system, particularly MedWatch, functions as a decentralized, patient-driven pharmacovigilance network that effectively leverages real-world evidence to detect signals that preclinical trials simply can't capture due to limited sample sizes and duration. The fact that 1.3 million adverse event reports are submitted annually speaks volumes about the collective vigilance of the healthcare ecosystem, and it's remarkable how even a dozen confirmed cases can trigger a regulatory response-this isn't reactive governance, it's adaptive science in action. The evolution toward genetic risk stratification, like HLA-B*57:01 for liver toxicity, represents a paradigm shift from population-level warnings to truly personalized risk communication. We're moving from ‘one-size-fits-all caution’ to ‘precision safety,’ which is not just medically sound but ethically imperative.
olive ashley December 8, 2025 AT 18:38
Black box warnings? Yeah right. Ever notice how every drug that gets one is always the one that’s cheaper than the alternatives? Coincidence? Or did the FDA get a kickback from the pharma giants to scare people into buying the $1,200/month ‘safer’ version? I’ve seen the reports. They’re edited. The truth? They don’t want you to know what’s really in the bottle.
Ibrahim Yakubu December 10, 2025 AT 09:56
Listen here, America. You think this is about safety? No. This is about control. The FDA doesn't care if you live or die. They care if you obey. They put the black box there so you'll be too scared to question. So you'll take your pills like a good little citizen. And when you die? They'll say, 'We warned you.' But they never warned you about the real danger-the system that lets them decide who lives and who doesn't.
Chris Park December 10, 2025 AT 15:06
You're all missing the point. The FDA doesn't add black box warnings because drugs are dangerous. They add them because lawsuits are expensive. The real killer isn't the drug-it's the lawyer who found the one patient who died. This is litigation-driven pharmacology, not science. The data is cherry-picked, the statistics inflated. And you people just nod along like sheep.
Priya Ranjan December 11, 2025 AT 06:07
It’s irresponsible to suggest that people should just ‘ask their doctor’-most doctors don’t even read the full prescribing information. They skim the summary and prescribe based on reps’ pitches. The burden shouldn’t be on the patient to dig up FDA documents. The warning should be on the bottle. Period.
Gwyneth Agnes December 12, 2025 AT 23:03
Stop taking drugs. Your body can heal itself.
Kay Jolie December 13, 2025 AT 19:58
It’s profoundly ironic that we’ve reached a point where the most potent pharmacological interventions require a literal black border to signify existential risk. The epistemological rupture between clinical utility and existential peril has never been more starkly visualized. The black box isn’t just a warning-it’s a semiotic monument to the collapse of therapeutic optimism. We’ve turned medicine into a risk calculus where hope is quantified in odds ratios and survival curves. And yet, we still cling to the illusion that the box is the problem, not the system that demands such boxes exist.
Clare Fox December 15, 2025 AT 05:16
It’s strange how we treat medicine like it’s supposed to be perfect. We want drugs to fix us without cost, without risk, without consequence. But life doesn’t work that way. The black box isn’t a flaw in the system-it’s a mirror. It shows us we’re not in control. That some choices have weight. That sometimes, the only way out is through the danger. Maybe the warning isn’t there to scare us… but to remind us we’re still alive enough to be afraid.
Akash Takyar December 17, 2025 AT 00:35
Dear friends, I urge you to approach black box warnings not with fear, but with disciplined curiosity. Each warning is a roadmap-crafted by years of suffering, data, and sacrifice. Please, do not dismiss them. Do not ignore them. Instead, treat them as sacred documents: print them, share them, discuss them with your provider. Keep a journal of symptoms. Schedule your bloodwork. Be the patient who asks, “What if?”-and then, “What next?” Your life is not a gamble. It is a covenant-with yourself, with your doctor, with science.
Andrew Frazier December 18, 2025 AT 02:25
So now the FDA’s the hero? Funny how they let every junk drug through for 20 years then slap a box on it when the lawsuits start rolling in. You think they care about you? Nah. They care about their budget. And your ignorance. Keep taking your pills, dumbass.