Most people don’t think about their bones until something breaks. But bone loss doesn’t come with pain, swelling, or warning signs. It’s silent. By the time a fracture happens - often from a simple fall or even a sneeze - the damage is already done. That’s why DEXA scan screening matters. It’s not just another test. It’s your best chance to catch weak bones before they fail.
Every year in the U.S., over 2 million fractures happen because of osteoporosis. Half of women over 50 and a quarter of men will break a bone in their lifetime due to low bone density. And here’s the scary part: 80% of those people never had a bone density test before their fracture. A DEXA scan isn’t about fear. It’s about control. If you know your numbers, you can act. If you don’t, you’re guessing.
What a DEXA Scan Actually Measures
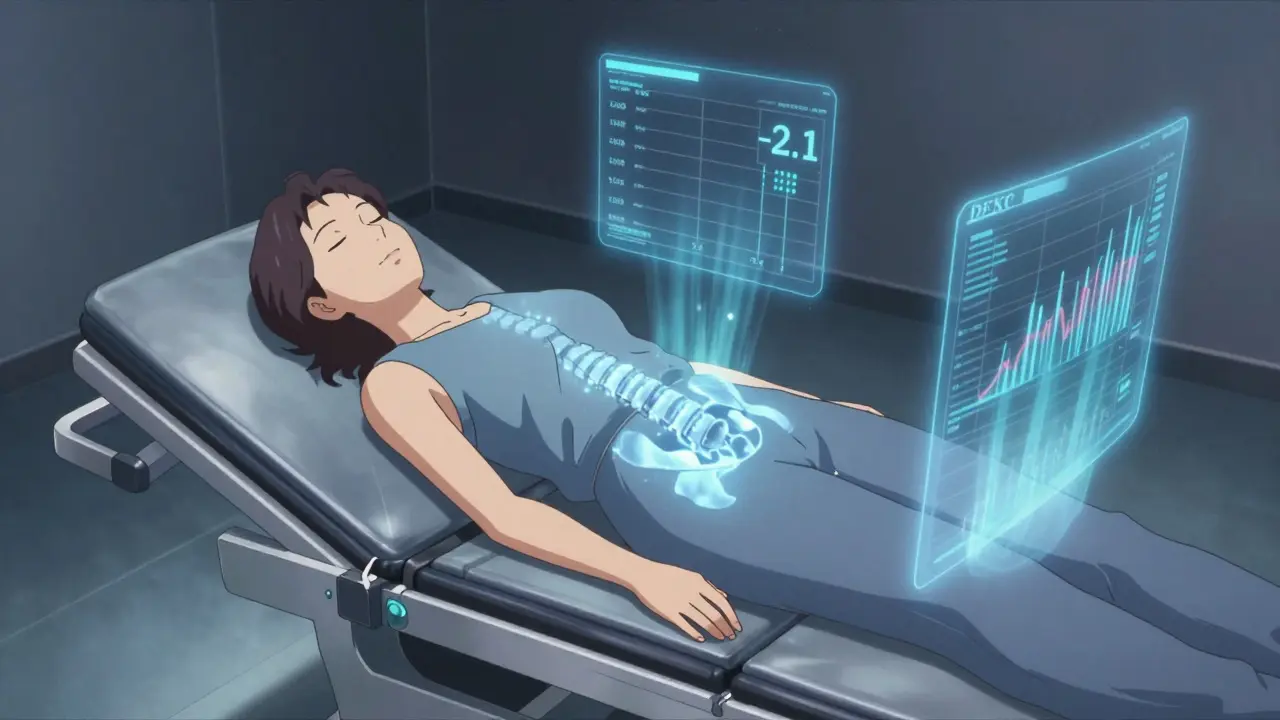
A DEXA scan - short for dual-energy X-ray absorptiometry - is the gold standard for checking bone strength. It uses two very low-dose X-ray beams to measure how much mineral is packed into your bones. The machine doesn’t take pictures like a regular X-ray. It calculates density in grams per square centimeter. That number tells you if your bones are dense enough to handle daily stress or if they’re thinning out.
The scan focuses on the two places most likely to break: the lower spine (lumbar vertebrae) and the hip. Sometimes, if you’ve had wrist fractures or joint replacements, they’ll also scan your forearm. The whole thing takes about 10 minutes. You lie on a table. The machine passes over you like a giant, quiet printer. No needles. No fasting. No discomfort. The radiation you get is less than what you’d absorb from a cross-country flight or two days of natural background radiation.
Understanding Your T-Score
Your DEXA report gives you one number that matters most: the T-score. This isn’t just a number. It’s your bone’s personal report card compared to a healthy 30-year-old adult of your same sex and ethnicity.
- T-score of -1.0 or higher: Normal bone density. Your bones are in good shape.
- T-score between -1.0 and -2.5: Osteopenia. Your bone density is below average but not yet osteoporosis. This is your wake-up call.
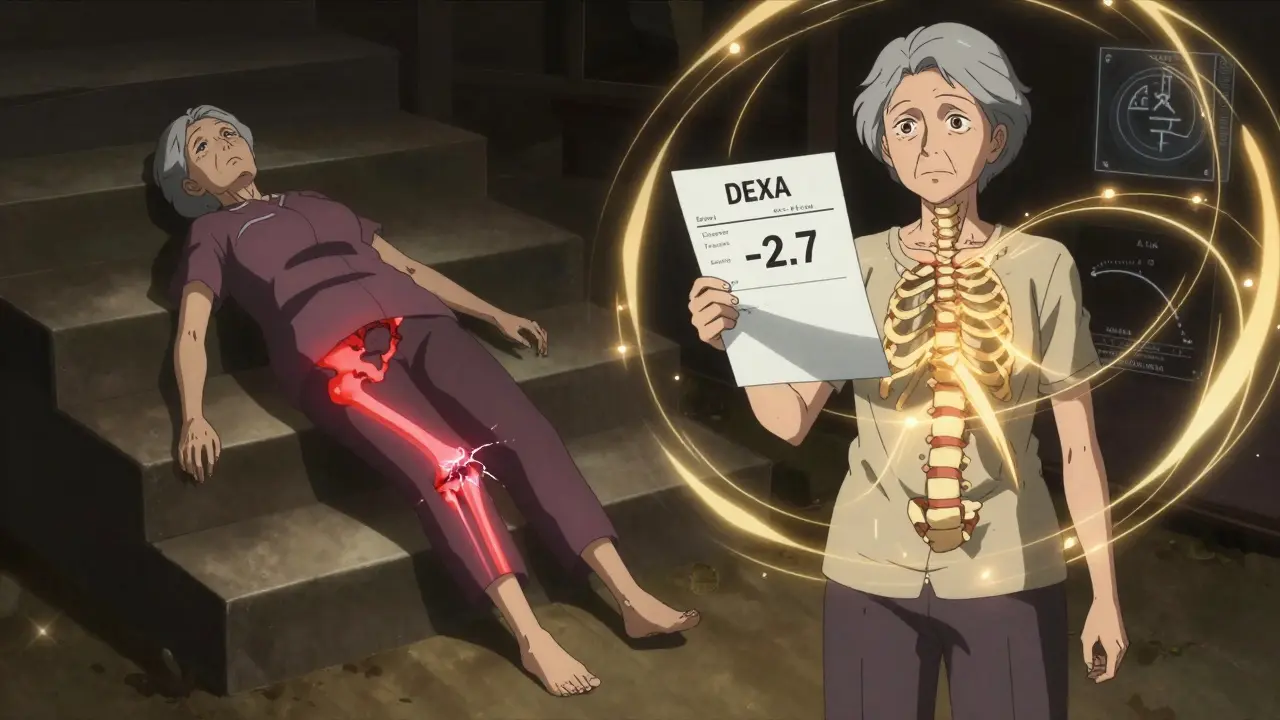
- T-score of -2.5 or lower: Osteoporosis. Your bones are fragile. Fracture risk goes up sharply.
Let’s say your T-score is -2.1. That’s osteopenia. It doesn’t mean you’ll break a bone tomorrow. But it does mean your risk is climbing. Studies show people with osteopenia are 2 to 3 times more likely to fracture than those with normal density. And if your T-score is -3.0? Your fracture risk jumps to 5 to 7 times higher.
Don’t confuse T-score with Z-score. Z-score compares you to people your own age. It’s useful for younger adults or those with unusual risk factors. But for most people over 50, the T-score is what doctors use to make decisions.
Fracture Risk Isn’t Just About Bone Density
Here’s the truth: a low T-score doesn’t tell the whole story. Some people with osteopenia break bones. Others with osteoporosis never do. Why? Because bone strength isn’t just about density. It’s about structure, balance, and lifestyle.
The FRAX tool was created by the World Health Organization to fix this gap. It takes your DEXA result and adds in your age, sex, weight, smoking status, alcohol use, family history of hip fracture, and whether you’ve had a prior fracture. It then calculates your 10-year chance of breaking a hip or other major bone.
For example: a 68-year-old woman with a T-score of -2.7 (osteoporosis) who never smoked, drinks one glass of wine a week, and has no family history might have a 12% fracture risk. But another woman with the same T-score who smokes, drinks heavily, and had a wrist fracture at 60? Her risk jumps to 34%. That’s not just a number. That’s a reason to start medication.
Studies in the Journal of Bone and Mineral Research show FRAX improves prediction accuracy by 15-22% over DEXA alone. That’s why doctors now use both.
Who Needs a DEXA Scan?
You don’t need a DEXA scan just because you’re over 50. But if you fit any of these categories, you should get one - and soon.
- Women 65 and older
- Men 70 and older
- Postmenopausal women under 65 with risk factors (low body weight, smoking, steroid use, family history)
- Men 50-69 with risk factors
- Anyone who broke a bone after age 50 from a minor fall
- People on long-term steroid medication (like prednisone for more than 3 months)
- People with rheumatoid arthritis, hyperthyroidism, or malabsorption disorders
Medicare covers DEXA scans every two years for eligible people. Most private insurers follow the same rules. If you’re unsure, ask your doctor. It’s not a luxury. It’s preventive care.
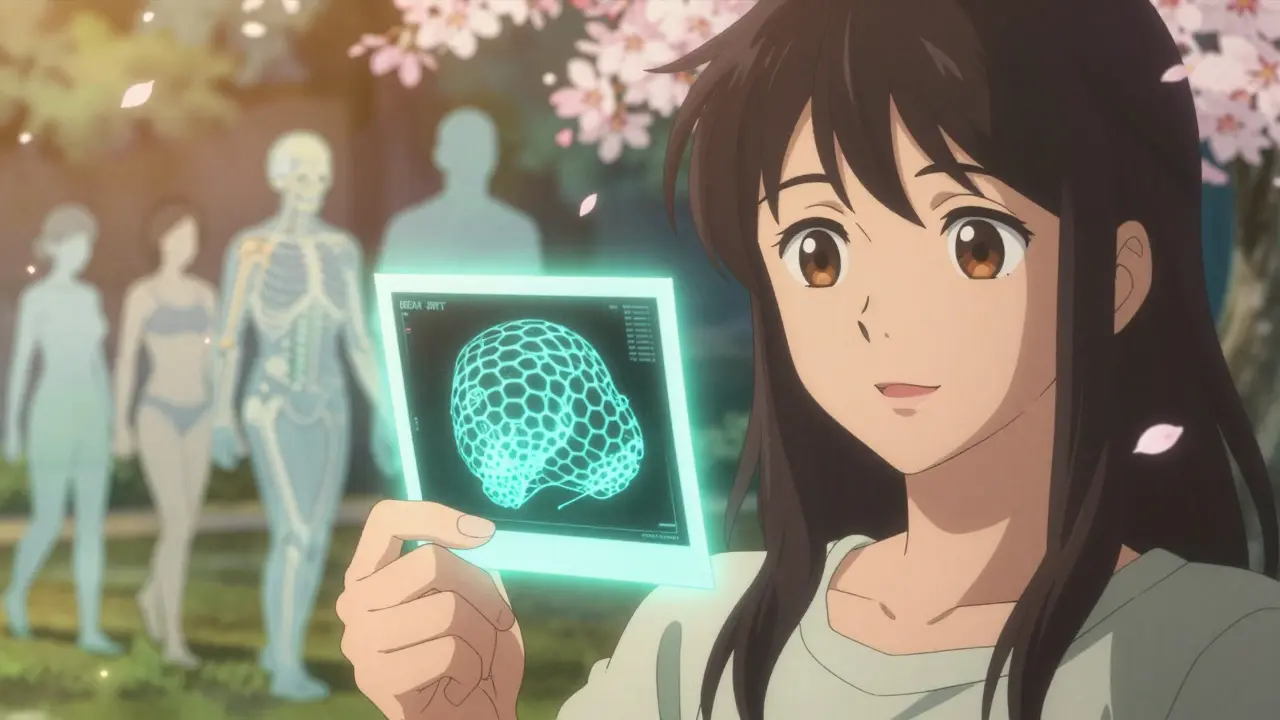
What DEXA Can’t Tell You
DEXA is powerful - but limited. It can’t see how your bone is structured inside. Two people can have the same T-score, but one has a honeycomb-like internal structure that’s strong. The other has thin, brittle rods that snap easily. That’s why some people fracture despite “normal” DEXA results.
New tools are starting to fix this. Trabecular Bone Score (TBS) analyzes the texture of your spine on the DEXA image. It doesn’t need extra radiation. It just uses the data already collected. Studies show TBS improves fracture prediction by 12-18%. It’s not yet standard everywhere, but more clinics are adding it.
Also, DEXA struggles with people who have severe arthritis, spinal fusion, or metal implants. The machine can’t tell if low density is from bone loss or from calcium deposits in nearby arteries. That’s why your technologist needs to be trained - and why you should go to a certified facility.
What Happens After the Scan?
If your scan shows normal bone density? Great. Keep doing what you’re doing. Eat enough protein. Get vitamin D. Walk daily. Avoid falls.
If you have osteopenia? You’re not helpless. Lifestyle changes can slow or even reverse bone loss. Weight-bearing exercise (like walking, dancing, or lifting weights) three times a week. 1,200 mg of calcium daily. 800 IU of vitamin D. Stop smoking. Cut back on alcohol. These steps can improve your T-score by 1-2% per year.
If you have osteoporosis? Medication is often needed. Drugs like alendronate (Fosamax), denosumab (Prolia), or teriparatide (Forteo) can reduce fracture risk by 40-70%. They’re not magic. But they work - if taken as prescribed.
One real case from the National Osteoporosis Foundation: a 68-year-old woman had a T-score of -2.7. She had no symptoms. No pain. No history of fractures. Her doctor recommended medication. She started it. Two years later, her repeat scan showed improvement. She never broke a bone. She didn’t know she was at risk - until the scan told her.
Common Misconceptions
- “I don’t need a scan because I’m not old enough.” Bone loss starts in your 30s. Women lose 1-2% of bone per year after menopause. Waiting until 65 means you’ve already lost 20-30%.
- “I’m not at risk because I’m healthy.” You can be fit, eat well, and still have low bone density. Genetics, hormones, and medications play bigger roles than you think.
- “The radiation is dangerous.” One DEXA scan equals less radiation than a day of sun exposure. You get more from driving to the clinic.
- “My doctor said I’m fine, so I don’t need one.” Many primary care doctors don’t routinely order DEXA scans unless you ask. Don’t wait for them to bring it up.
What to Do Next
Don’t ignore bone health until it’s too late. If you’re over 50 - or under 50 with risk factors - talk to your doctor about a DEXA scan. Ask for your T-score. Ask about FRAX. Don’t settle for vague answers like “you’re fine.”
Take action now. Whether it’s starting calcium, walking more, or getting medication - knowing your numbers gives you power. And power means you can keep living without fear of breaking.
What is a normal DEXA scan result?
A normal DEXA result means your T-score is -1.0 or higher. This means your bone density is within 1 standard deviation of a healthy young adult. You don’t have osteopenia or osteoporosis. But that doesn’t mean you can ignore bone health - bone loss starts early, and prevention matters.
Can I get a DEXA scan if I have a pacemaker or metal implants?
Yes, but it may affect accuracy. Pacemakers and joint replacements don’t block the scan, but they can create shadows on the image, especially in the hip or spine. The technician will note this, and your doctor may skip the affected area or use alternative sites like the forearm. Always tell the tech about any implants before the scan.
How often should I get a DEXA scan?
If your first scan is normal or shows mild osteopenia and you’re not on treatment, repeat every 5 years. If you have osteoporosis or are on medication, repeat every 1-2 years to track progress. Medicare and most insurers cover scans every two years for eligible people. More frequent scans are only needed if your risk changes - like starting steroids or having a fracture.
Do I need to prepare for a DEXA scan?
No special prep is needed. Don’t take calcium supplements 24 hours before the scan. Wear loose clothing without metal zippers or buttons. If you’ve had a barium study or CT scan with contrast in the last 10 days, reschedule - the leftover contrast can interfere with results. Otherwise, just show up.
Is DEXA better than a regular X-ray for detecting bone loss?
Yes. A regular X-ray only shows bone loss after you’ve lost 30% or more. DEXA detects changes as small as 1-2%. That means it catches problems years before a fracture happens. DEXA is the only test approved by the U.S. Preventive Services Task Force for routine osteoporosis screening.


9 Comments
Logan Hawker February 15, 2026 AT 21:55
Let’s be real-the DEXA scan is the only diagnostic modality that actually quantifies bone mineral density with precision, right? I mean, we’re talking about dual-energy X-ray absorptiometry here, not some amateurish radiographic approximation. The T-score isn’t just a number-it’s a standardized Z-score normalized against peak bone mass in young adults, and frankly, if your clinician isn’t using FRAX in tandem, you’re getting suboptimal care. And don’t even get me started on how underutilized TBS is-texture analysis of trabecular architecture? It’s the future. Yet most clinics still treat DEXA like a binary yes/no test. Pathetic.
James Lloyd February 16, 2026 AT 03:55
I’ve reviewed hundreds of DEXA reports over the years, and one thing stands out: people fixate on the T-score like it’s a final verdict. But bone health isn’t a spreadsheet-it’s a living system. Weight-bearing exercise, vitamin K2, magnesium, and protein intake matter just as much as the scan. I had a patient with a T-score of -2.3 who never fractured because she lifted weights three times a week and ate fermented dairy daily. Meanwhile, another with a -1.8 broke her hip after tripping over a rug. Density isn’t destiny. Structure, balance, and daily habits are.
Digital Raju Yadav February 16, 2026 AT 18:44
Why are Americans so obsessed with scanning themselves to death? In India, we don’t need fancy machines to know if your bones are weak-you can see it in how people walk, how they hunch over, how they avoid stairs. We’ve been managing osteoporosis for centuries with diet, sunlight, and ayurvedic herbs like ashwagandha and shatavari. Your entire healthcare system is built on fear, profit, and overtesting. One scan costs $300? That’s robbery. And now you’re all scared to sneeze because some machine told you your bones are ‘osteopenic.’ Pathetic.
Carrie Schluckbier February 17, 2026 AT 18:00
Have you ever wondered why DEXA scans are pushed so hard right after menopause? Coincidence? Or is Big Pharma quietly funding guidelines to sell bisphosphonates? I’ve read the studies-many of them are funded by drug manufacturers. And let’s not forget: the FDA approved Prolia knowing it could cause jaw necrosis and atypical femur fractures. They just didn’t tell you. Your ‘preventive care’ is a trap. They want you dependent on drugs for life. Your bones don’t need chemicals-they need sunlight, movement, and truth.
Liam Earney February 18, 2026 AT 15:31
It’s fascinating, really, how we’ve reduced the profound, complex phenomenon of skeletal integrity down to a single, cold, numerical metric-the T-score-as if bone health were a standardized test score from high school. But bones aren’t math. They’re not static. They’re dynamic, responsive, alive, shaped by gravity, by movement, by sleep, by stress, by the rhythm of the seasons, by the quality of the soil in which our food was grown. And yet, we’ve outsourced our bodily wisdom to a machine that hums quietly while we lie still, trusting its algorithm more than our own intuition. Isn’t that tragic? And isn’t that exactly how modern medicine has turned us all into passive consumers of our own biology?
guy greenfeld February 20, 2026 AT 02:31
What if the real problem isn’t osteoporosis… but the illusion of control? We think we can quantify bone strength like we can quantify IQ or cholesterol. But life isn’t a spreadsheet. You can have a T-score of -0.8 and fall from a ladder and break your pelvis. You can have a T-score of -3.5 and hike the Appalachian Trail at 75. The scan gives you a number. It doesn’t give you meaning. It doesn’t give you courage. It doesn’t tell you whether you’ve lived hard enough, loved deeply enough, moved boldly enough to have earned strong bones. Maybe the real fracture isn’t in the hip-it’s in how we’ve stopped trusting our bodies and started trusting machines.
Adam Short February 21, 2026 AT 16:43
Let’s not sugarcoat this: the UK’s NHS has been dragging its feet on DEXA access for years. We’ve got elderly people in rural areas waiting 18 months for a scan while their bones crumble. Meanwhile, the Americans are out here with their $300 scans and FRAX calculators and TBS add-ons-like it’s some kind of tech conference. We need universal access, not a luxury service for the insured. And if you’re telling me that a woman in rural Wales can’t get screened because she’s ‘not high risk’-that’s not healthcare. That’s neglect dressed up as policy. We need to stop treating bone health like a secondary concern. It’s a public health emergency.
Sam Pearlman February 23, 2026 AT 05:37
Okay but what if I told you DEXA scans are actually kinda useless for men? Like, the whole ‘T-score compared to a 30-year-old’ thing was designed for women, right? Men don’t have menopause, so their bone loss is slower, more gradual. But we still get labeled ‘osteoporotic’ at -2.5 even if we’ve been lifting weights since high school. I’ve got a T-score of -2.8 and I deadlift 300. My bones are fine. The machine doesn’t know that. It just sees a number. So now I’m being pushed into meds I don’t need. Thanks, medicine.
Steph Carr February 24, 2026 AT 21:34
My grandmother broke her hip at 89. She never had a DEXA scan. She danced tango every Sunday until she was 85. She ate eggs, drank milk from a cow, and walked barefoot in the garden. She didn’t take calcium pills. She didn’t know what FRAX was. She just lived. And you know what? She never complained. I think we’ve forgotten that bones aren’t just made of calcium-they’re made of joy, movement, sunlight, and the quiet dignity of showing up for life. Maybe the real screening tool isn’t a machine. Maybe it’s whether you still want to get up and dance.