Bariatric Surgery Medication Adjuster
Adjust Your Medication Dose
Calculate appropriate dose adjustments for medications after bariatric surgery based on your surgery type and medication class.
What Happens to Your Medications After Bariatric Surgery?
When you have bariatric surgery, your body doesn’t just lose weight-it changes how it handles everything you swallow, including your medicines. The stomach gets smaller. Parts of the intestine get bypassed. Digestion speeds up. And suddenly, pills that used to work perfectly might not work at all. This isn’t speculation. It’s a well-documented clinical reality. Studies show that up to 68% of people who’ve had Roux-en-Y gastric bypass need to adjust their medications within the first year. For sleeve gastrectomy patients, it’s still around 32%. The problem isn’t just about taking more pills. It’s about whether the medicine even reaches your bloodstream the way it’s supposed to.
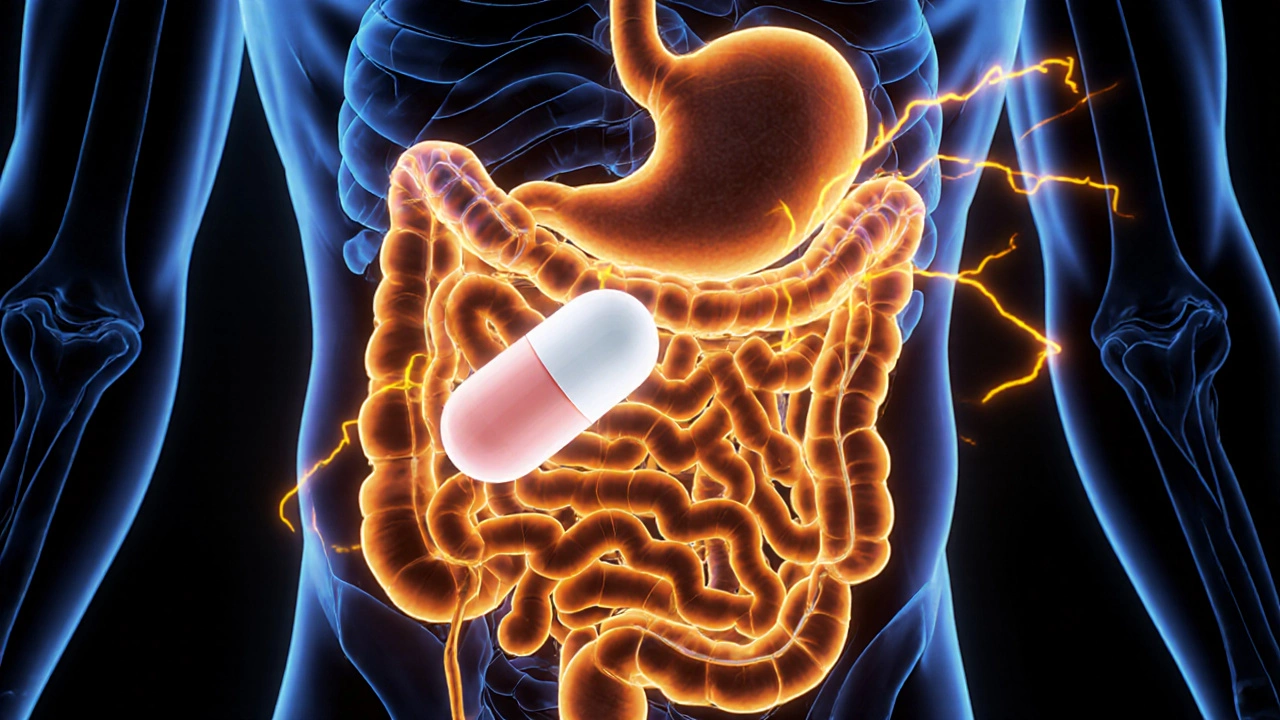
Why Your Pills Don’t Work the Same Way Anymore
Your digestive system is a carefully designed drug delivery system. Before surgery, a pill sits in your stomach for a couple of hours. Acid breaks it down. Then it moves slowly through the duodenum and jejunum, where most drugs are absorbed. After surgery, that whole process gets scrambled. In a gastric bypass, up to 150 centimeters of your small intestine-where critical drugs like calcium, iron, and levothyroxine are absorbed-are skipped entirely. Your stomach is now the size of an egg. The pH rises from 2 to 5, making it harder for acid-dependent drugs to dissolve. And instead of spending hours moving through your gut, everything rushes through in under an hour.
This isn’t just theory. In one study, patients who took extended-release metformin after gastric bypass had 30-40% lower blood levels. Glipizide XL lost nearly 75% of its effectiveness. Oxycodone CR was only 40% as potent. These aren’t rare cases. They’re predictable outcomes based on anatomy.
Not All Surgeries Are the Same
Not every bariatric procedure affects drug absorption the same way. The type of surgery you had matters more than you think.
- Roux-en-Y Gastric Bypass (RYGB): This is the big one. It bypasses the duodenum and part of the jejunum. About 70% of patients need medication changes. Extended-release pills often fail completely. Acid-dependent drugs like ketoconazole or atazanavir become unreliable. Iron and calcium absorption drops by 35%. Levothyroxine needs a 25-30% dose increase in most cases.
- Sleeve Gastrectomy: This one removes most of the stomach but leaves the intestines untouched. Absorption is less disrupted-around 85% of normal remains. But because the stomach is so small, large pills may not dissolve properly. Gastric pH still rises, which can affect drugs like atazanavir or rilpivirine. Dose changes are less frequent, but still needed in 15-20% of cases.
- Biliopancreatic Diversion with Duodenal Switch: This is the most extreme. It bypasses nearly two-thirds of the small intestine. Bioavailability for many drugs drops by 50-70%. This procedure is rare (only 2.5% of cases), but if you’ve had it, you’re at the highest risk for medication failure.
- Adjustable Gastric Banding: Minimal impact on anatomy. The main issue? You eat less. If your medicine needs food to be absorbed-like mycophenolate-you might need a higher dose because you’re not eating enough.
Which Medications Are Most at Risk?
Some drugs are more sensitive to these changes than others. These are the ones that cause the most trouble:
- Extended-release (ER) and delayed-release pills: These are designed to release slowly over hours. After bypass surgery, they zip through your system too fast. The drug doesn’t have time to dissolve. Glipizide XL, metformin ER, and oxycodone CR are common examples. Most experts recommend switching to immediate-release versions.
- Acid-dependent drugs: These need stomach acid to dissolve. After surgery, your stomach is less acidic. Drugs like ketoconazole, itraconazole, and atazanavir lose effectiveness. Some patients need to take them with acidic drinks like orange juice or switch to liquid forms.
- Calcium, iron, and vitamin B12: These are absorbed in the bypassed areas. Even with supplements, many patients still become deficient. Calcium citrate is preferred over calcium carbonate because it doesn’t need acid to absorb.
- Levothyroxine: This thyroid hormone is absorbed in the upper small intestine. After RYGB, 41% of patients need higher doses. Some need to switch from tablets to liquid or gel caps. Taking it on an empty stomach helps-22% better absorption in one study.
- Anticoagulants like warfarin: Even small changes in absorption can be dangerous. Warfarin levels can drop by 25-35% after RYGB. One study found 60% of patients needed higher doses. Weekly INR checks are required for the first 3 months.
- Antiepileptics and immunosuppressants: These have narrow therapeutic windows. A small drop in blood levels can mean seizures or organ rejection. Therapeutic drug monitoring is mandatory.
What Should You Do? A Practical Guide
If you’ve had bariatric surgery, here’s what you need to do right now:
- Review every medication with your pharmacist. Don’t wait for a problem. Bring your full list-prescription, OTC, supplements-to a pharmacist who understands bariatric changes. Many community pharmacists haven’t been trained for this.
- Switch ER pills to immediate-release. If you’re on metformin ER, glipizide XL, or similar, ask your doctor about switching. A 1:1.25 conversion ratio is common (e.g., 500mg ER becomes 625mg immediate-release, split into two doses).
- Use liquids or crushable forms when possible. For the first 3-6 months, liquid or chewable forms are safest. If you must take pills, make sure they’re small and easy to dissolve. Avoid large, hard tablets.
- Take meds at the right time. Acid-dependent drugs? Take them 30-60 minutes before meals. Food-dependent drugs? Take them with a meal. Levothyroxine? Take it on an empty stomach, at least 30 minutes before food or coffee.
- Get blood tests. For warfarin, levothyroxine, phenytoin, and immunosuppressants, regular blood level checks are not optional. Weekly at first, then monthly or quarterly depending on stability.
- Track your symptoms. Did your pain meds stop working? Did your thyroid symptoms come back? Did your blood sugar spike? These aren’t coincidences. They’re signs your meds aren’t being absorbed.
What’s New in Medication Management?
Things are changing fast. In 2024, the European Medicines Agency required all new oral drugs to include bariatric surgery absorption data. The FDA added warnings to 17 drug labels. Pharmacies are hiring specialized bariatric pharmacists-200% more since 2018. And new tech is emerging:
- PH-adaptive capsules: These are designed to dissolve even in low-acid environments. Early trials show 85% absorption in post-surgery patients-compared to 45% for regular pills.
- Subcutaneous implants: For diabetes, drugs like exenatide can now be delivered through a small implant under the skin. One 2023 study found 92% effectiveness in RYGB patients, versus 68% with oral versions.
- AI dosing calculators: Eighty-three U.S. hospitals now use AI tools that factor in your surgery type, weight, and drug history to recommend doses. They’ve cut dosing errors by 41%.
What Patients Are Saying
Reddit threads in r/bariatricsurgery are full of stories. One user, PostOpPharmD, shared that his levothyroxine dose jumped from 75mcg to 125mcg after RYGB. Another said his antidepressants stopped working-until he switched from tablets to liquid. A third described how his blood thinner didn’t work for months, and he nearly had a stroke. These aren’t outliers. They’re the rule.
The NHS tracked 142 adverse drug reactions in bariatric patients between 2018 and 2022. Over half involved blood thinners. Nearly a quarter involved diabetes meds. The most common complaints? "Pills won’t dissolve," "meds don’t work," and "I have to take more pills now."
Don’t Guess. Get Tested.
There’s no one-size-fits-all answer. Your surgery type, your weight, your age, your other meds-all of it matters. The key is not to assume your old doses still work. Don’t wait for a crisis. Talk to your pharmacist. Get your blood tested. Switch your pills if needed. This isn’t about being paranoid. It’s about staying alive. Medication absorption after bariatric surgery isn’t a minor detail. It’s a medical priority. And if you’re not being monitored for it, you’re being put at risk.
What’s Next?
More research is coming. Mayo Clinic is now testing pharmacogenomics-using your genes to predict how you’ll absorb drugs after surgery. If your CYP enzymes metabolize drugs slowly, your dose might need to be lower, even if your anatomy suggests higher. This could be the future: personalized medicine based on both your genes and your gut.
For now, the rule is simple: if you’ve had bariatric surgery, your meds are different. Treat them that way.
Do all bariatric surgeries affect medication absorption the same way?
No. Roux-en-Y gastric bypass causes the most significant changes because it bypasses parts of the small intestine where many drugs are absorbed. Sleeve gastrectomy mainly reduces stomach size, so absorption is less affected. Gastric banding has minimal impact on anatomy but can reduce food intake, which affects drugs that need food to be absorbed. Biliopancreatic diversion causes the most severe malabsorption.
Can I still take extended-release pills after bariatric surgery?
Generally, no. Extended-release pills are designed to dissolve slowly over hours. After surgery, especially gastric bypass, the pills move through your system too quickly and don’t release properly. Most experts recommend switching to immediate-release versions. For example, metformin ER should be replaced with regular metformin taken twice daily.
Why does my thyroid medicine not work after surgery?
Levothyroxine is absorbed in the upper small intestine, which is bypassed in Roux-en-Y gastric bypass. This can reduce absorption by 25-30%. Many patients need a 20-40% dose increase. Taking it on an empty stomach, 30-60 minutes before food, improves absorption. Some patients benefit from switching to liquid or gel cap forms.
Should I get blood tests for my medications after surgery?
Yes-if you take drugs with a narrow therapeutic window. This includes warfarin, phenytoin, levothyroxine, immunosuppressants, and some antidepressants. Blood levels can change dramatically after surgery. For warfarin, weekly INR checks are recommended for the first 3 months. Don’t assume your old dose is still safe.
What should I do if my pain meds aren’t working after surgery?
If you’re taking extended-release opioids like oxycodone CR, they’re likely not being absorbed properly. Studies show up to 60% reduced bioavailability. Ask your doctor to switch to immediate-release oxycodone or another short-acting option. You may need a higher dose or more frequent dosing. Never increase the dose on your own.
Are there new types of pills designed for bariatric patients?
Yes. Researchers are developing pH-adaptive capsules that dissolve even in higher stomach pH levels, which are common after surgery. One type showed 85% absorption efficiency compared to 45% for standard pills. Subcutaneous implants, like the exenatide device, bypass the gut entirely and are proving highly effective. These aren’t widely available yet, but they’re the future of post-bariatric medication.


13 Comments
Neoma Geoghegan November 23, 2025 AT 20:01
ER pills are a trap after RYGB. Switched my metformin to immediate-release and my A1C dropped 2 points in 6 weeks. No more guessing.
Bartholemy Tuite November 23, 2025 AT 22:04
bro i thought my meds were just being lazy after surgery but nope. my oxycodone cr went from 10mg every 8hrs to needing 15mg every 4hrs and still felt nothing. switched to immediate-release and now i can actually sit down without crying. also learned the hard way that calcium carbonate is useless now. citrate only. thank god for that pharmacist who actually knew what she was talking about.
Sam Jepsen November 25, 2025 AT 16:45
Just had my 18mo post-op check and my endo finally caught my levothyroxine was still at 75mcg. After RYGB, my TSH was 8.5. They bumped me to 112mcg. Within 2 weeks, my energy came back. I was a zombie before. Don’t wait for symptoms to get bad. Get tested. Get educated. This isn’t optional.
Yvonne Franklin November 26, 2025 AT 10:06
Warfarin after bypass is a minefield. My INR dropped to 1.1 after 3 months. Almost had a PE. Now I’m on weekly checks. Liquid forms of meds saved me too. No more swallowing giant pills. My pharmacist even got me a pill cutter that works on enteric coatings. Life changing.
Michael Fitzpatrick November 27, 2025 AT 11:15
It’s wild how much your body changes after surgery. I didn’t realize my antidepressants stopped working until I started crying for no reason at work. Switched from tablets to liquid sertraline and suddenly I could breathe again. Also took me 6 months to figure out my iron supplement wasn’t working because I was taking the wrong kind. Calcium carbonate = useless. Citrate = magic. Wish I’d known this sooner.
Shawn Daughhetee November 29, 2025 AT 06:50
my pill crush game is strong now. everything gets crushed or switched to liquid. even my gabapentin. no more giant capsules that just sit in my stomach like rocks. and yeah i take my levothyroxine on an empty stomach like a boss. no coffee no food no nothing. 30 mins before. its a ritual now. and my tsh is perfect. thanks to the pharmacist who actually listened.
Miruna Alexandru November 29, 2025 AT 09:39
It’s not just absorption-it’s pharmacokinetics. You’re altering the Cmax, Tmax, and AUC of every drug by rerouting GI transit time and gastric pH. The fact that most clinicians still treat this as an afterthought is alarming. We’re not talking about minor fluctuations. We’re talking about subtherapeutic dosing leading to clinical failure. This isn’t anecdotal. It’s biologically deterministic. And yet, most patients are left to figure it out on their own. The system is broken.
Justin Daniel November 30, 2025 AT 07:23
lol i used to think i was just ‘bad at taking meds’ until i found out my extended-release pills were just shooting right through me like a bullet. now i take everything with water, on an empty stomach, and i’ve got a little checklist taped to my fridge. levothyroxine before coffee. iron with orange juice. warfarin with food. it’s weird but it works. also, thank you to whoever wrote this post. i finally feel seen.
Mark Williams December 1, 2025 AT 17:27
PH-adaptive capsules are the future. Saw a trial at my hospital-85% absorption vs 45% for standard. That’s not a marginal gain. That’s a paradigm shift. And subcutaneous exenatide? Game changer for RYGB diabetics. No more relying on a gut that’s been surgically reconfigured. We’re moving from ‘adapt your body’ to ‘adapt your delivery.’ This is precision medicine meeting bariatric reality.
David Cunningham December 2, 2025 AT 07:41
my pain doc said ‘just take more’ when my oxycodone stopped working. i did. got dizzy. almost fell down stairs. then i found a bariatric pharmacist. switched to immediate-release. doubled the frequency. now i can walk my dog without feeling like i’m on a rollercoaster. also, never take calcium carbonate again. i learned that one the hard way.
luke young December 2, 2025 AT 16:23
so many people don’t realize this is a thing. i had my sleeve 3 years ago and only found out last year that my gabapentin wasn’t working because of my stomach size. switched to liquid. boom. no more nerve pain at night. also, i take my iron with vitamin c now. it’s wild how simple fixes can be if you know where to look.
james lucas December 4, 2025 AT 03:02
just wanted to say thank you to the author. i was about to quit my meds because i thought they were just ‘not for me’ but then i read this and went to my pharmacist. turned out my glipizide xl was basically useless after my bypass. switched to regular, split the dose, and my sugars are stable for the first time in 2 years. also, i crush all my pills now. no shame. it works.
Jessica Correa December 4, 2025 AT 15:44
my thyroid meds stopped working after surgery and i thought it was stress or depression. turns out my dose needed to go up 30%. got tested, switched to gel caps, took it on empty stomach. now i’m not tired all the time. also, calcium citrate is the only kind that works. i learned that from a Reddit thread. never underestimate the power of patient communities.