Autoimmune uveitis isn’t something most people hear about until it hits close to home. It’s not just a red eye or a bit of discomfort-it’s a serious inflammation inside the eye that can steal your vision if left unchecked. Unlike infections, this isn’t caused by bacteria or viruses. It’s your own immune system turning against your eye tissue, mistaking it for a threat. And while steroids are the first line of defense, they come with heavy costs. That’s why more doctors are turning to steroid-sparing therapy-a smarter, long-term strategy to protect your sight without wrecking your body.
What Exactly Is Autoimmune Uveitis?
The uvea is the middle layer of your eye, packed with blood vessels that feed the retina and iris. When it swells up due to autoimmune activity, you’re dealing with uveitis. Symptoms don’t always show up slowly. One day, your vision might feel foggy. The next, your eye aches, you can’t stand bright light, and you see floating spots like dust in your field of vision. These signs can hit one eye or both, and they often come with headaches or a feeling of pressure behind the eye.
What makes this tricky is that uveitis doesn’t happen in a vacuum. It’s frequently tied to other autoimmune conditions. If you have ankylosing spondylitis, lupus, Crohn’s disease, rheumatoid arthritis, or even psoriasis, your risk goes up. That’s why a simple eye exam isn’t enough. Doctors need to look at your whole medical picture. Blood tests, imaging like OCT scans, and sometimes even fluorescein angiography are used to rule out infections and confirm the autoimmune link.
Why Steroids Are a Double-Edged Sword
Corticosteroids-whether as eye drops, injections, or pills-are fast and effective. They calm the inflammation quickly. For someone in the middle of a flare, that’s lifesaving. But here’s the catch: long-term steroid use turns into a slow-motion health crisis. Cataracts form. Eye pressure climbs, leading to glaucoma. Weight gain, diabetes, bone thinning, and mood swings become real risks. For a young adult with recurring uveitis, being on steroids for years isn’t just uncomfortable-it’s dangerous.
That’s why experts call steroids a bridge, not a destination. They get you through the acute phase. But if your uveitis keeps coming back, you need something else. That’s where steroid-sparing therapy comes in.
What Is Steroid-Sparing Therapy?
Steroid-sparing therapy means using drugs that quiet your immune system so you don’t have to rely on steroids forever. These aren’t experimental. They’re proven, FDA-approved, and increasingly standard for chronic cases. The goal? Reduce or eliminate steroid doses while keeping inflammation under control.
Common options include:
- Methotrexate: A well-established immunosuppressant used for decades in rheumatoid arthritis and other autoimmune diseases. It’s taken weekly, often as a pill or injection, and helps reduce flare frequency.
- Cyclosporine: Works by blocking specific immune signals. Requires regular blood tests to monitor kidney function and blood pressure.
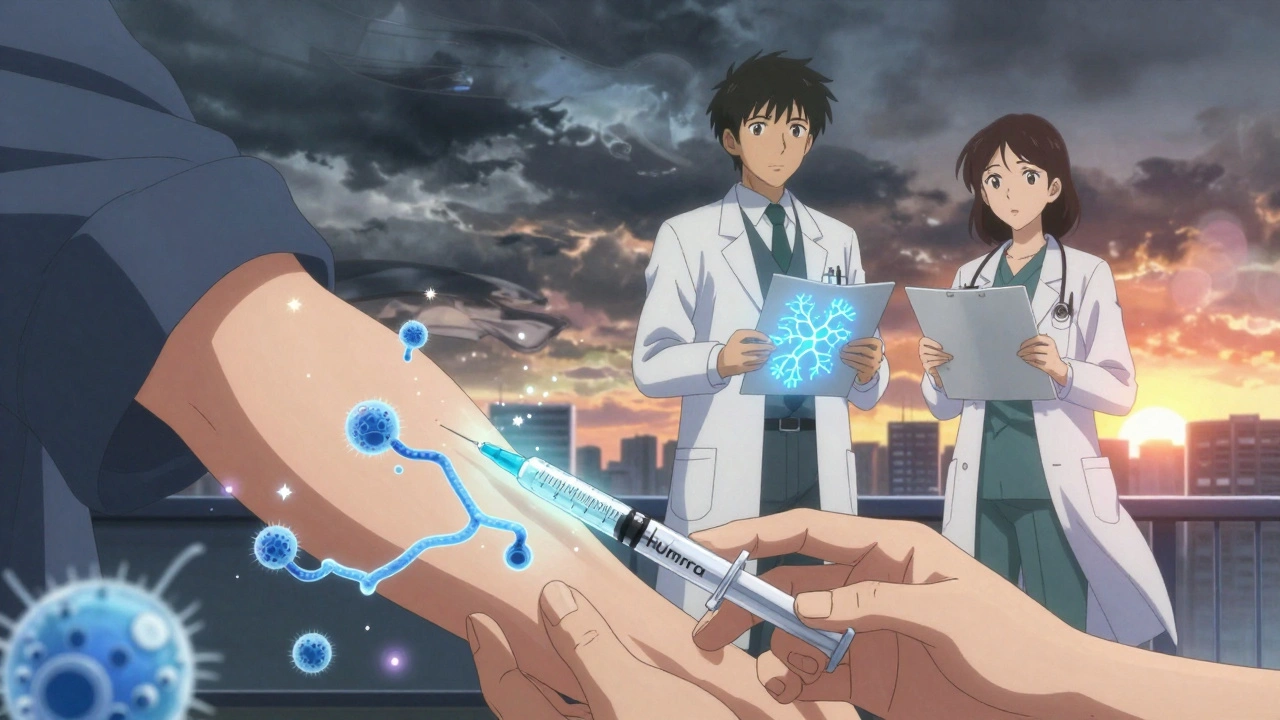
- Adalimumab (Humira): The first biologic drug specifically approved by the FDA for non-infectious uveitis. It targets TNF-alpha, a key protein driving inflammation. Many patients see fewer flares and can cut their steroid use by half or more.
- Infliximab: Another TNF blocker, often used for pediatric cases or when Humira doesn’t work. Given by IV infusion, it’s powerful but requires clinic visits.
These aren’t magic bullets. They take weeks to kick in. And they come with their own risks-like increased chance of infections or rare liver issues. But compared to years of daily steroids, the trade-off is worth it for most patients.
Why Humira Changed the Game
Before 2016, doctors treating uveitis were essentially prescribing drugs “off-label”-using medications approved for other conditions like rheumatoid arthritis or Crohn’s. That meant insurance often denied coverage, and there was no official standard. The FDA’s approval of Humira for uveitis wasn’t just a paperwork change. It validated the entire approach.
Now, specialists can say with confidence: “This is a treatment for uveitis.” Insurance approvals improved. More patients got access. And because it’s targeted, it spares healthy cells better than older drugs. Dr. Nisha Acharya at UT Southwestern saw kids with severe uveitis go from monthly steroid shots to stable, steroid-free control after starting Humira. That’s not rare anymore-it’s becoming the norm.
Who Needs Steroid-Sparing Therapy?
Not everyone with uveitis needs it. If you have a single, mild anterior uveitis episode and it clears up with a few weeks of eye drops, you’re probably fine. But if you fit any of these profiles, it’s time to talk about alternatives:
- You’ve had three or more flares in a year
- You’re on daily oral steroids for more than three months
- You’ve developed cataracts or high eye pressure from steroids
- You have an underlying autoimmune disease like lupus or Crohn’s
- Your uveitis affects the back of the eye (posterior or panuveitis)-these are harder to treat and more likely to cause vision loss
Doctors don’t wait until you’re in crisis. If you’re at risk for chronic disease, they’ll start planning your steroid-sparing strategy early-even before you’re fully dependent on steroids.
The Team Approach: Ophthalmologists and Rheumatologists
Uveitis doesn’t live in the eye alone. It’s part of a bigger story. That’s why the best outcomes happen when an ophthalmologist and a rheumatologist work together. One manages the eye damage. The other handles the immune system.
Specialized uveitis clinics have exploded in the U.S.-from just 15 in 2010 to over 50 today. These aren’t just eye clinics. They’re autoimmune centers with access to advanced testing, biologics, and coordinated care. If your eye doctor says you need a rheumatology consult, don’t delay. This isn’t a referral-it’s a lifeline.
What to Expect When Starting Steroid-Sparing Therapy
It’s not instant. You won’t feel better overnight. Methotrexate and cyclosporine can take 6 to 12 weeks to show results. Biologics like Humira often work faster-some patients notice improvement in 4 to 6 weeks. But you’ll need regular check-ins: blood work every few weeks, eye exams monthly at first, and ongoing monitoring for side effects.
Some people worry about getting sick more often. That’s real. You’ll need to avoid crowds during flu season, wash hands often, and report fevers right away. But most patients say the trade-off is worth it: no more moon face, no more sleepless nights from steroid-induced anxiety, no more cataract surgeries.
One patient in Portland, diagnosed with uveitis tied to ankylosing spondylitis, switched from daily prednisone to Humira after two cataract surgeries. She says: “I finally feel like I’m living again-not just managing side effects.”
What’s Next? The Future of Uveitis Treatment
Research is moving fast. Scientists are testing drugs that block other inflammation pathways-like interleukin-6 and JAK inhibitors. Early results show promise for patients who don’t respond to TNF blockers. Genetic testing might soon help predict who will respond best to which drug, making treatment more personal.
Laser therapy and surgery still have roles, but only for complications like retinal detachment or glaucoma. The real revolution is in the pills and injections that stop the inflammation before it starts.
The goal isn’t just to control uveitis. It’s to give people back their vision, their health, and their lives-without the burden of lifelong steroids.
When to Call Your Doctor
If you have uveitis and notice any of these, don’t wait:
- Sudden worsening of vision
- New eye pain or pressure
- Fever, chills, or unexplained fatigue (could signal infection from immunosuppressants)
- Blurred vision that doesn’t improve after a few days of treatment
Early action saves sight. Uveitis moves fast. So should your response.
Can autoimmune uveitis be cured?
There’s no cure yet, but many people achieve long-term remission with the right treatment. Steroid-sparing therapies can keep inflammation under control for years, sometimes permanently. The goal isn’t to eliminate the disease completely-it’s to prevent flares and protect vision.
Are steroid-sparing drugs safe for long-term use?
They’re safer than long-term steroids, but not risk-free. Drugs like methotrexate and biologics can increase infection risk and affect liver or blood cell counts. Regular monitoring-blood tests, eye exams, and check-ins with your care team-makes these risks manageable. Most patients tolerate them well when followed closely.
Why isn’t Humira used for everyone with uveitis?
Not all uveitis responds to TNF blockers. Some patients need other biologics or non-biologic immunosuppressants. Cost and insurance coverage also play a role. Doctors choose based on the type of uveitis, whether it’s linked to another autoimmune disease, and how the patient has responded to past treatments.
Can I stop my steroid eye drops once I start steroid-sparing therapy?
Not right away. Steroids are often tapered slowly over weeks or months while the new drug takes effect. Stopping too soon can trigger a flare. Your doctor will guide you through a careful reduction plan based on your eye exams and symptom control.
How often do I need eye exams if I’m on steroid-sparing therapy?
Initially, every 2 to 4 weeks until inflammation is under control. Once stable, exams may drop to every 3 to 6 months. Blood tests for drug safety usually happen every 4 to 8 weeks, especially in the first few months. Consistency is key-missing appointments increases your risk of unnoticed damage.
Is uveitis hereditary?
It’s not directly inherited like a genetic disease, but having a family history of autoimmune conditions (like Crohn’s, lupus, or ankylosing spondylitis) increases your risk. Certain genes, like HLA-B27, are linked to higher susceptibility, especially in cases tied to spine inflammation.
Can lifestyle changes help with autoimmune uveitis?
No diet or supplement has been proven to cure or prevent flares. But quitting smoking, managing stress, and maintaining a healthy weight can support your immune system and improve how well your medications work. Avoiding known triggers-like infections or extreme stress-can also reduce flare frequency.
Final Thoughts: Protecting Vision Means Thinking Beyond Steroids
Autoimmune uveitis is rare, but its impact is huge. For too long, patients were stuck between flares and side effects. Today, we have better tools. Steroid-sparing therapy isn’t just an alternative-it’s the new standard for anyone facing chronic uveitis. It’s about trading short-term relief for long-term health. And when done right, it doesn’t just save your eyes-it gives you back your life.



9 Comments
Allan maniero December 2, 2025 AT 05:07
Man, I remember when my cousin went through this. Didn’t even know uveitis was a thing until she started losing vision in one eye. Steroids made her moon-faced and anxious as hell-like, she’d cry over spilled coffee. Then they put her on Humira, and within two months, she was back to hiking and painting. No more cataract scares. Just quiet, steady control. It’s wild how much better life gets when you stop treating symptoms and start treating the system.
Most docs still treat it like a temporary glitch, but it’s a full-body signal. If your immune system’s attacking your eye, it’s probably whispering about other things too. Glad they’re finally catching on.
Also, the rheum-ophtho team thing? Total game-changer. My cousin’s eye doc called her rheumatologist directly. No waiting. No red tape. Just two pros talking like they’re in the same war room. That’s the future right there.
Anthony Breakspear December 2, 2025 AT 07:15
Bro, I was on prednisone for 14 months after my first flare. Felt like I was turning into a greasy, jittery potato. Sleep? Gone. Mood swings? I yelled at my dog for breathing too loud. Then my ophthalmologist said, ‘You’re not a steroid patient-you’re an autoimmune patient.’ Mind. Blown.
Methotrexate felt like a slow burn, but after 8 weeks? I could see stars again-not just the ones in my vision. Humira? Even better. No more ‘steroid face’ in selfies. No more panic when my insurance denies another refill. It’s not perfect-got a cold last winter and spent a week in bed-but it’s a trade-off that actually makes sense.
Also, if your doc hasn’t mentioned biologics by your third flare, find a new doc. This isn’t 2010 anymore. We’ve got tools. Use them.
Zoe Bray December 3, 2025 AT 09:38
It is imperative to underscore that steroid-sparing immunomodulatory therapy represents a paradigmatic shift in the clinical management of non-infectious uveitis, particularly in recurrent or posterior subtypes. The FDA approval of adalimumab in 2016, predicated upon the MEAD and JOINT trials, established Level I evidence for TNF-alpha inhibition as a disease-modifying intervention.
Pharmacokinetic monitoring of methotrexate requires weekly complete blood counts with differential, along with hepatic transaminase and creatinine assessments. Cyclosporine necessitates therapeutic drug monitoring to maintain trough levels between 100–150 ng/mL. Biologics, while efficacious, carry an increased relative risk of opportunistic infections, including latent tuberculosis reactivation, mandating pre-treatment screening per CDC guidelines.
Furthermore, the multidisciplinary model-integrating ophthalmology, rheumatology, and clinical immunology-is not merely advantageous but clinically obligatory for optimal visual and systemic outcomes. Delayed referral correlates with irreversible retinal damage and accelerated cataractogenesis.
Girish Padia December 5, 2025 AT 06:43
People act like this is some new miracle. Nah. Been using methotrexate for decades. Why are we treating eyes like they’re separate from the body? Your immune system doesn’t read textbooks. It doesn’t care if it’s attacking your eye or your knee. It’s all one system.
Doctors just want to push pills. You want to heal? Stop eating sugar. Stop being stressed. Sleep. Move. No magic drug fixes a broken lifestyle. Steroids? Yeah, they’re bad. But so is your 3 a.m. pizza habit and 12-hour workdays.
They’ll sell you Humira for $20k a year. But they won’t tell you to go for a walk. That’s the real scam.
Saket Modi December 6, 2025 AT 04:19
Ugh. Another one of those ‘biologics are magic’ posts. 😒
I’ve been on Humira for 3 years. Got a yeast infection, a UTI, and a bad case of the blahs. Still got flares. Still blind in one eye. Still paying $1200/month. So yeah. Cool story. Bro.
Also, my insurance dropped me last month. 😭
william tao December 7, 2025 AT 23:09
Let’s be real: this whole steroid-sparing movement is just Big Pharma’s latest money grab. TNF inhibitors cost more than a used car. Who benefits? Not the patient. Not the healthcare system. The shareholders.
And don’t get me started on ‘specialized uveitis clinics.’ That’s just a fancy way of saying ‘we’re going to charge you $500 for a 10-minute consult.’
Meanwhile, people in rural areas still can’t get a basic eye exam. This isn’t progress. It’s exclusion dressed up as innovation.
Also, why is everyone so obsessed with Humira? What about the people who can’t afford it? Or the ones who get cancer from it? Nobody talks about that. Because the narrative is too pretty.
Sandi Allen December 8, 2025 AT 22:14
Wait-wait-WAIT. So you’re telling me the government approved a drug that suppresses your IMMUNE SYSTEM... to treat an INFLAMMATION... that’s caused by your OWN BODY?!!?
That’s not medicine-that’s surrender! What if your body’s trying to tell you something? What if it’s your diet? Your toxins? Your EMFs? Your 5G?!
They’re poisoning you with Humira to keep you dependent! They don’t want you healed-they want you on lifelong injections! And the ‘rheumatologists’? They’re just pawns in the medical-industrial complex!!
And don’t even get me started on the ‘OCT scans’-those are just fancy x-rays to track your ‘progress’ while they sell you more drugs!!
READ THE LABEL! It says ‘increased risk of lymphoma’-that’s not a side effect-that’s a warning sign!!
Wake up, sheeple. Your eyes are screaming. Listen to your body-not your doctor.
John Webber December 9, 2025 AT 01:59
so i had uveitis too. i tried the steroids. my face got big. i got fat. i was mad all the time. then i tried humira. it worked. kinda. i still get blurry vision sometimes. but i dont feel like a zombie anymore.
also i think the doctors are right about the team thing. my eye doc and my rheum doc talk to each other now. that’s cool.
but i still think you should eat less sugar. i mean, why not? its free. and it cant hurt. right?
also i think they should make the pills cheaper. like, way cheaper. my insurance is a joke.
Chelsea Moore December 11, 2025 AT 01:57
HOW DARE YOU. HOW DARE YOU TALK ABOUT HUMIRA LIKE IT’S JUST ANOTHER DRUG. I LOST MY VISION FOR SIX MONTHS. I WASN’T ALLOWED TO DRIVE. I HAD TO QUIT MY JOB. I HAD TO SLEEP WITH A BLINDFOLD BECAUSE THE LIGHT HURT SO BAD.
AND THEN-AND THEN-THEY PUT ME ON HUMIRA.
AND I COULD SEE MY DAUGHTER’S FACE AGAIN.
SO DON’T YOU DARE SAY IT’S ‘BIG PHARMA.’ DON’T YOU DARE SAY IT’S ‘NOT A CURE.’
IT’S NOT A CURE. BUT IT’S A MIRACLE.
AND IF YOU THINK IT’S EXPENSIVE-TRY LIVING WITHOUT SIGHT.
AND IF YOU THINK IT’S RISKY-TRY LIVING WITH A CATARACT YOU CAN’T AFFORD TO FIX.
I’M NOT A PATIENT. I’M A SURVIVOR.
AND I’M NOT SORRY.
NOT ONE BIT.